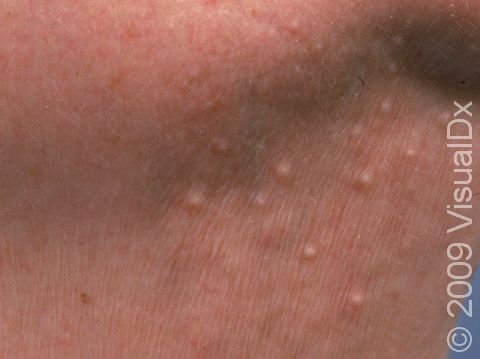
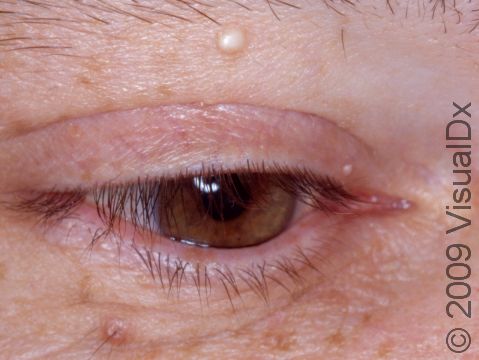
Milia
Milia are commonly found on the skin of people of all ages. They are formed when keratin (a substance produced by the skin) becomes entrapped beneath the outer layer of the skin, forming a tiny cyst (an enclosed lump underneath the skin). An individual milium (the singular of milia) is formed at the base of a hair follicle or sweat gland.
Milia can be categorized as either primary or secondary. Primary milia are formed directly from entrapped keratin and are usually found on the face of infants or adults. Secondary milia look similar, but they develop after something clogs the ducts leading to the skin surface, such as after an injury, burn, or blistering of the skin.
Who's At Risk?
Milia can occur in people of any age, race / ethnicity, or sex. Primary milia are especially common in newborns (occurring in up to 50% of newborns).
Secondary milia may appear in affected skin of people with:
- Burns.
- Blistering injury to skin, such as poison ivy.
- Blistering skin conditions, such as bullous pemphigoid, epidermolysis bullosa, and porphyria cutanea tarda.
- Skin resurfacing procedures such as dermabrasion or laser resurfacing.
- Long-term use of steroid creams.
- Chronic sun damage.
Signs & Symptoms
Milia appear as 1-2 mm white-to-yellow, dome-shaped cysts that are not painful or itchy.
The most common locations for milia in adults are the cheeks, eyelids, nose, chin, forehead, and genital skin.
Milia in adults may last for months or years.
Self-Care Guidelines
Milia in adults tend to be long-lasting, but they may go away on their own.
Although milia are found in the outer layers of skin, they are difficult to remove without the proper tools. Do not try to remove them at home, as you may leave a scar.
Treatments
Milia do not require treatment. However, in the case of secondary milia, the medical professional will want to treat any underlying skin condition. For people who would like to have milia removed, your medical professional may treat milia with one of the following:
- Piercing each milium with a sterile blade or scalpel followed by removal of the keratin with a tool called a comedone extractor
- Topical retinoid cream such as tretinoin, tazarotene, or adapalene
- A series of acid peels or microdermabrasion procedures at the dermatologist’s office
Visit Urgency
See a medical professional for evaluation if you notice any new cysts on the skin.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 18th, 2024 at 8:31 am

Not sure what to look for?
Try our new Rash and Skin Condition Finder