
Excessive Sweating (Hyperhidrosis)
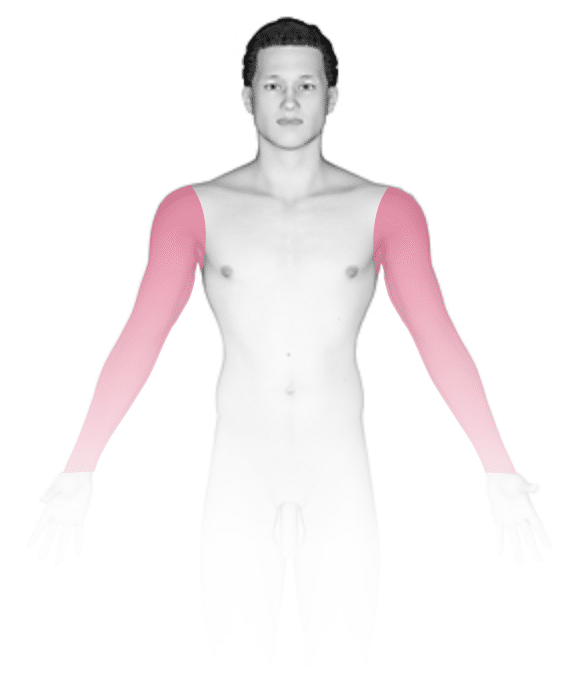
Hyperhidrosis, the medical name for excessive sweating, involves overactive sweat glands, usually in body parts such as the palms, soles, forehead, or underarms. Sometimes, though, hyperhidrosis can be generalized, affecting the majority of the skin, and uncommonly it may be caused by an underlying medical condition. Hyperhidrosis can be quite debilitating, depending on the extent and location of the symptoms. Social and professional interactions can be affected due to fear of embarrassment caused by sweating in front of others.
Who's At Risk?
Excessive sweating most often presents in childhood or adolescence, although it can start in adults as well. In up to half of people, there may be a family history of this condition, or it can also be seen in association with certain diseases or medications.
Signs & Symptoms
Excessive sweating can develop during certain emotional states, such as in stressful conditions, or in response to triggers such as spicy foods, alcohol, or lotions.
Self-Care Guidelines
The following self-care measures can help:
- Avoiding triggers that lead to hyperhidrosis (eg, spicy foods, stressful situations)
- Using “clinical strength” antiperspirants that are available over the counter (eg, Secret, Dove, Certain Dri)
- Using products for excessive sweating specifically on the feet (eg, Certain Dri Foot Powder)
- Using an antiperspirant-deodorant combination for the prevention of odor in addition to sweating
- Wearing loose-fitting clothing made from natural fabrics to wick away moisture from areas of sweating and allow for faster drying of the skin
- Keeping your environment cool
- Support groups for people with hyperhidrosis, including the International Hyperhidrosis Society and Hyperhidrosis UK
Treatments
If there is an underlying condition or medication causing your hyperhidrosis, the medical professional will aim to identify what it is and help resolve the cause. Your medical professional will look through your medication list to see if there are any that may be triggering the condition.
There are several common treatments that can be tried to reduce the impact of symptoms of excessive sweating, depending on what body location(s) are affected:
- Topical treatments containing aluminum compounds or glycopyrrolate act by blocking the sweat glands.
- Glycopyrrolate and oxybutynin are oral medications that block molecules involved in signaling between the nervous system and the sweat glands.
- Iontophoresis involves the passage of electric current into the skin to disrupt the functioning of the sweat glands. This is most easily used for the palms and soles. Some units can be purchased for use at home.
- Botulinum toxin injection (Botox) is used to inhibit signaling between the nervous system and the muscle fibers found in the sweat glands.
- Sympathectomy is a surgical procedure used as a last attempt to control symptoms. The nerves of the sympathetic nervous system (those that govern the sweating behavior) are cut to reduce symptoms. Unfortunately, side effects such as excessive sweating in previously unaffected areas (known as compensatory hyperhidrosis) can result.
Visit Urgency
If you have generalized hyperhidrosis or hyperhidrosis that is accompanied by other symptoms, such as flushing, headaches, diarrhea, weight loss, or weight gain, seek medical care to ensure there is no underlying medical condition causing it. Consultation with a medical professional should be sought when over-the-counter antiperspirants / deodorants are not effective in controlling symptoms. If symptoms are debilitating, causing major lifestyle changes such as avoiding social situations for fear of embarrassment, seek consultation with a medical professional such as a dermatologist.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 17th, 2024 at 3:04 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder


