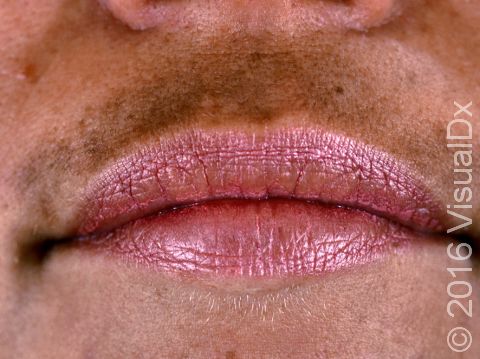
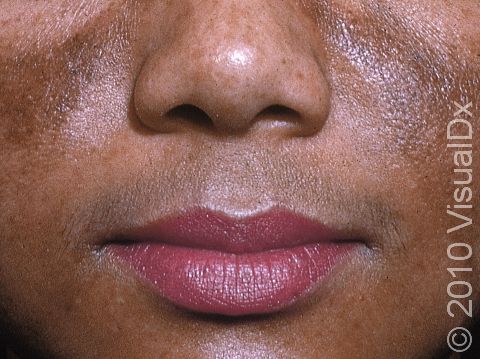
Melasma
Melasma is a common disorder that causes dark patches, often on sun-exposed areas of the face. The brown patches of melasma worsen in response to increases of the hormone estrogen, such as during pregnancy or with the use of birth control pills. Other medications, such as antiseizure medications, may also cause melasma. Increased sun exposure can also be a cause.
Who's At Risk?
Although the condition is more common in women, men can also have melasma.
People with darker skin colors get melasma more often than those with lighter skin colors.
Signs & Symptoms
Patches of melasma most commonly affect the face, particularly the cheeks, forehead, upper lip, and nose. In darker skin colors, melasma is any shade of brown, including dark brown. In lighter skin colors, it may be tan or light brown.
Self-Care Guidelines
- Protect your skin from sun exposure to prevent worsening of melasma, and use sunscreen on all exposed skin areas, including the lips, before going outdoors. A broad-spectrum sunscreen (meaning it blocks UVB and UVA light) with sun protection factor (SPF) of at least 30 is best. Avoid spray sunscreens as they do not provide a thick enough layer of protection; use a lotion or cream sunscreen. Tinted sunscreens provide the most protection against melasma.
- Use sunscreen year-round as the skin is very sensitive to even small amounts of ultraviolet (UV) light.
- Cover-up makeups, such as Dermablend, may mask the condition.
Treatments
Your medical professional may recommend:
- A bleaching agent (eg, hydroquinone 4%). Do not apply bleaching agents to the normal surrounding skin as normal skin may also be bleached. Use hydroquinone under the supervision of a medical professional as side effects, such as darkening of the skin, may occur if taken for long periods.
- A combination cream formulation of hydroquinone 4%, fluocinolone acetonide 0.01%, and tretinoin 0.05% (nightly for 8-24 weeks).
- Superficial chemical peels (application of an acid to remove the top layers of the skin) and microdermabrasion (a facial sanding technique).
- Creams such as azelaic acid and kojic acid.
- Laser therapy and an oral medication, tranexamic acid.
Visit Urgency
Melasma is a harmless condition that does not require treatment, but if it becomes bothersome, see your medical professional. If you suspect your melasma is caused by a medication you are taking, talk to your medical professional about potentially stopping or switching medications.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 14th, 2024 at 3:35 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder