Heat Rash or Prickly Heat (Miliaria Rubra)
Miliaria rubra, commonly known as heat rash or prickly heat, is a common skin condition caused by the blockage of sweat ducts that carry sweat from sweat glands to the skin surface. Although this rash can be caused by fever, heat rash is more commonly seen in infants who are dressed too warmly.
Who's At Risk?
Heat rash is common in overbundled infants in the winter and those who have recently moved to a hot, humid climate.
Signs & Symptoms
Heat rash may appear as tiny papules (solid bumps) or vesicles (fluid-filled blisters, also known as miliaria crystallina) surrounded by areas of red skin.
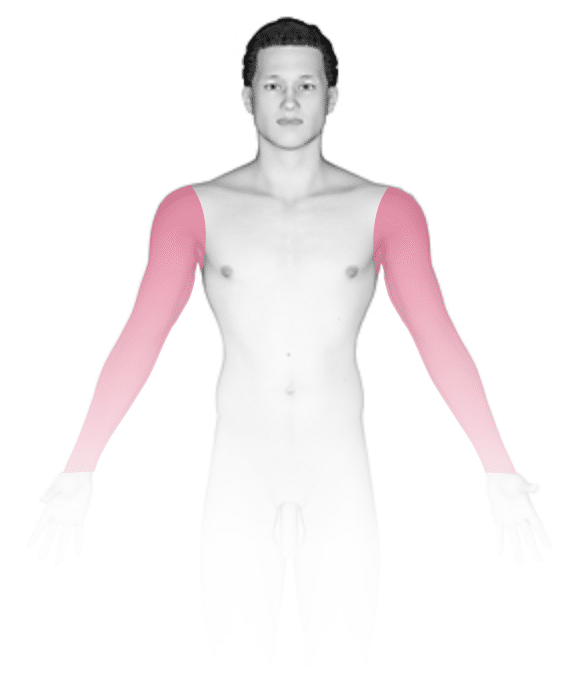
In infants, heat rash tends to occur on the upper trunk, back, neck, or in skinfolds such as the underarms.
Self-Care Guidelines
Prevention and treatment of heat rash consists of controlling heat and humidity. If there is a fever associated with the heat rash, you can give the infant acetaminophen (Tylenol) or ibuprofen (Motrin, Advil) to help reduce fever. Remove any tight clothing, limit the baby’s activity, and seek air conditioning or any cooler environment. Cool compresses can also help with the discomfort. The rash typically goes away on its own within weeks. Young infants should not be given fluids other than breast milk or formula unless instructed by a medical professional.
Treatments
If there are signs of bacterial skin infection related to the heat rash or otherwise, topical antibiotics may be given.
Dehydration may be treated with intravenous fluids, especially if there is vomiting. Heatstroke is treated by trying to quickly reduce the core temperature to normal. Immersion, evaporative, or invasive cooling techniques may be used in addition to rapid administration of intravenous fluids.
Visit Urgency
Typically, heat rash will resolve with self-care measures and no medical care is necessary. However, two complications of heat rash include secondary infection from scratching and heat exhaustion.
Seek medical care if your infant is scratching significantly. There are medications that can help relieve the itching and, thus, prevent infection. Infected areas may need antibiotics. Call the child’s medical professional if the area develops pus, redness, crusting, swelling, or tenderness.
In cases of heat exhaustion, the skin will appear hot and flushed without any sweat. The baby may seem listless or have difficulty breathing. This can progress to heatstroke, so urgent medical care should be obtained right away. Symptoms of heatstroke include a very high temperature of 105°F (40.56°C) or greater, decreased or loss of consciousness, or seizure.
Heat intolerance is recognized by a lack of sweating of the affected skin, irritable behavior, and a change in alertness. Call for emergency medical help if your infant shows one or more of the following symptoms:
- Your baby is sweaty and restless, then suddenly lethargic and sleepy. If your baby is awake, they may seem sort of limp or go from flushed to pale.
- Your baby shows signs of dehydration: a dry mouth, no tears with crying, cracked lips, sunken eyes, or has only 1 wet diaper every 6-8 hours.
- A decreased desire or ability to feed.
- Vomiting.
- Seizure.
- Fever.
If you notice some combination of these signs, do everything you can to cool off the baby and have them seen by a medical professional right away.
- Get your child into the shade or into an air-conditioned space.
- Undress your child and apply cool compresses.
- Do not give fluids.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on June 18th, 2024 at 8:59 am
Not sure what to look for?
Try our new Rash and Skin Condition Finder

