Bedsores (Pressure Ulcers)
Bedsores, also known as pressure ulcers, pressure injuries, pressure sores, and decubitus ulcers, result from prolonged pressure that cuts off the blood supply to the skin, causing the skin and other tissue to die. The damage may occur in as little time as 12 hours of pressure, but the visible damage may not appear until days later, once the skin begins to break down. The affected skin can open after pressure if it is exposed to further rubbing (friction) and/or moving the skin in one direction and the body in another (shear), as in sliding down when the bed head is raised. Dampness (such as from perspiration or incontinence) makes the skin even more susceptible to developing bedsores.
Who's At Risk?
People who cannot move themselves are at the greatest risk of getting bedsores, including people with:
- Spinal cord injury.
- Paralysis.
- Stroke.
- Nerve (neurologic) disease.
- Decreased mental awareness.
Most bedsores occur in people older than 70, as the skin of older people may be thinner and, when injured, it often heals more slowly.
People in nursing homes and hospitalized people (particularly for hip fracture or intensive care) develop bedsores more commonly.
Smokers and people who are malnourished or undernourished, have incontinence (problems with bladder or bowel control), diabetes, or problems with blood flow (circulation) also are at increased risk.
Signs & Symptoms
A bedsore appears first as a reddened area of skin that then breaks down to form an open, raw, oozing wound (ulcer).
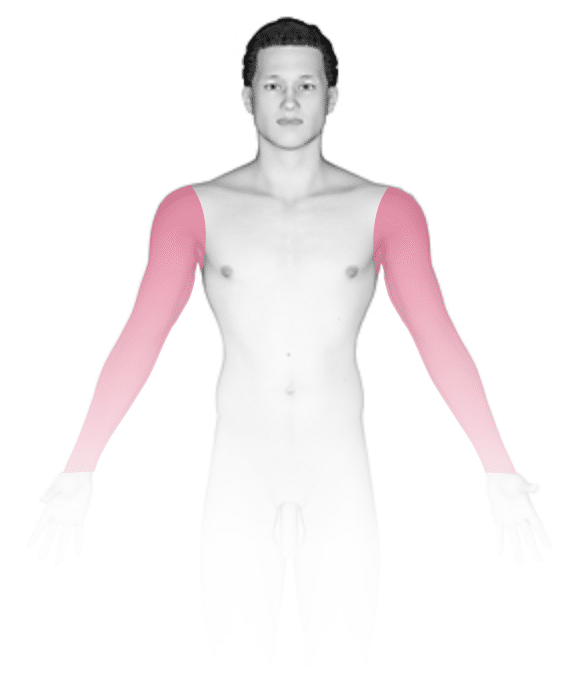
Bedsores occur at areas of abnormal pressure on the body:
- In a wheelchair, this is usually the tailbone (coccyx) or buttocks area, shoulder blades, spine, or backs of the arms or legs.
- In a bed, they may occur on the back of the head, ears, shoulder blades, hips, lower back, tailbone, or the backs or sides of the knees, elbows, ankles, or toes.
The pain level associated with bedsores depends on whether or not there is feeling in the area.
Bedsores occur in stages:
- Stage 1 has unbroken but pink or ashen (in darker skin colors) discoloration with perhaps slight discomfort or tenderness. In individuals with darker skin colors, there may be subtle discoloration in the area, or there may just be an area of warmth, a thickened area of skin, or an area of skin that feels harder than the surrounding skin.
- Stage 2 has red, swollen skin with a blister or open area(s).
- Stage 3 has a crater-like ulcer extending deeper into the skin.
- Stage 4 extends to deep fat, muscle, or bone and may have a thick black scab (eschar).
Self-Care Guidelines
Do not attempt self-care for any bedsore beyond stage 2 in appearance.
In the early stages (1 and 2) of bedsores, the area may heal with relief of pressure and by applying effective skin care (see below) to the affected skin.
A good diet will aid skin healing, especially by taking in enough vitamin C and zinc, which are available as supplements.
For effective skin care:
- If the skin is not broken, gently wash the area with mild soap and water.
- Gently clean open sores on the skin with salt water (saline), which can be made by boiling 1 quart of water with 1 teaspoon of salt for 5 minutes, then allowing it to cool.
- Apply a thin layer of petroleum jelly (Vaseline) and then cover with a soft gauze dressing.
- Keep urine and stool away from affected areas.
To relieve pressure:
- Change positions often (every 15 minutes in a chair and every 2 hours in a bed).
- Use special soft materials or supports (pads, cushions, and mattresses) to reduce pressure against the skin.
Treatments
- In addition to self-care, your medical professional may prescribe special pads or mattresses to help relieve pressure at the ulcer site(s).
- Special dressings may be used to cover the bedsores.
- Whirlpool baths or surgery may be recommended to remove dead tissue.
- Infection requires antibiotic treatment.
- Sometimes deep wounds may require surgery to restore the tissue.
Visit Urgency
If a stage 2 bedsore does not begin to heal in a few days or if the sore is at stage 3 or higher, seek medical advice.
Seek immediate care if you notice signs of infection (fever, spreading redness, swelling, or pus).
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on October 31st, 2023 at 12:28 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder





