Scabies
Scabies is a skin condition caused by a tiny mite called Sarcoptes scabiei. Scabies is very contagious and spreads rapidly in households and in crowded areas such as hospitals, nursing homes, childcare facilities, and other locations where people spend extended periods of time in close contact with one another.
The rash of scabies is extremely itchy and develops when a mite burrows into the skin and lays eggs. The human immune system is very sensitive to the presence of the mite and produces an allergic response that causes intense itching. Although a person who is infested with scabies usually only has 10-20 mites on their entire body, there may be a large number of lesions because of this allergic response. Without proper medical treatment, the condition will not usually improve.
Who's At Risk?
Scabies is seen in people of all races / ethnicities, ages, sexes, and at all socioeconomic levels. The infestation is not caused by lack of personal hygiene but is more frequently seen in people who live in crowded urban conditions.
Although scabies is extremely contagious, it usually requires prolonged skin-to-skin contact with a person who is infested. Limited contact, such as a hug or handshake, will not normally spread the infestation. Less commonly, scabies may be spread by sharing personal objects, such as towels, clothing, or bedding.
Scabies is easily spread to sexual partners and to members of the same household. Even people with scabies who do not have symptoms can pass the infestation on to other people.
Signs & Symptoms
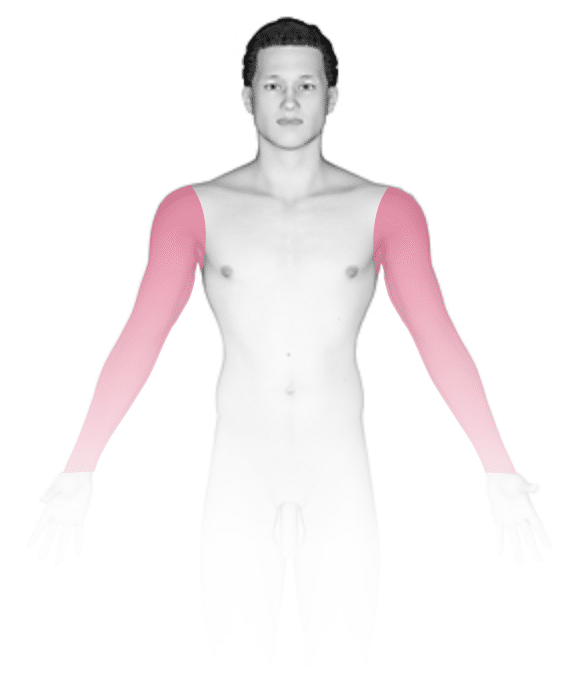
Although the entire body may itch, the most common locations for the lesions of scabies include the:
- Areas between the fingers (finger webs).
- Inner wrists, inner elbows, and armpits.
- Breasts of females and genitals of males.
- Belly button.
- Lower abdomen.
- Buttocks.
- Backs of the knees.
Although in adults it is rare to see lesions from scabies on the face, scalp, and neck, these areas are commonly affected in children aged younger than 2 years.
The most obvious signs of scabies are pink-to-red papules (small, solid bumps), sometimes with scale or a scab on them. In darker skin colors, the redness may be harder to see, or it may appear purple or brown. The telltale sign of scabies is the burrow, which is a small, thread-like, scaly line (3-10 mm long), sometimes with a tiny black speck (the burrowing mite) at one end. The adult mite is about 0.3 mm long and is very difficult to see.
People who are exposed to scabies may not develop itchy lesions for up to 6 weeks after becoming infested, as the immune system takes some time to develop an allergic response to the mites. However, individuals who have had scabies before may develop the rash within several days of re-exposure.
The rash of scabies is intensely itchy, especially at night. Excessive scratching of the itchy lesions can create breaks in the skin, which may then become infected with bacteria.
A severe form of scabies called crusted scabies is sometimes seen, especially in:
- Older adults.
- Individuals with weakened immune systems (such as organ transplant recipients or people with HIV / AIDS).
- People who are malnourished.
- People who are physically and/or mentally impaired or disabled.
In people with crusted scabies, the skin is covered with thick, white scales and crusts. The lesions are widespread, appearing over the scalp, face, elbows, knees, palms, and soles of the feet. Interestingly, these infestations may not be itchy, although the lesions may contain up to 2 million mites.
Self-Care Guidelines
Scabies requires prescription medication to treat the infestation. Once you have started treatment, there are steps you can take to remove scabies mites from the household and prevent reinfestation:
- Mites cannot survive off the human body for more than 48-72 hours. Therefore, wash all clothing, bedding, and towels used by the infested person in the past 72 hours in hot water, and dry these items in a hot dryer.
- Vacuum all carpets, rugs, and furniture, and discard the vacuum bags.
- Put anything that cannot be laundered into plastic bags for at least 72 hours.
Household pets do not need to be treated because the mite only lives on humans.
Treatments
Your medical professional may be able to diagnose scabies simply by examining your skin for typical lesions, such as burrows. They may also test for scabies by gently scraping some skin onto a slide and looking with a microscope for mites, eggs, or mite feces.
In most cases of scabies, your medical professional will prescribe a medicated cream or lotion to kill the infestation, such as:
- Permethrin cream, which is the first choice for treatment because it is very effective and safe. It is even safe for children and pregnant individuals. Apply to the entire body from the neck down. Smear the product beneath the fingernails and toenails. Apply to body folds, including inside the belly button, in the buttocks crease, and between the fingers and toes.
In more severe cases of scabies, your medical professional may prescribe an oral medication, such as:
- Ivermectin (eg, Stromectol) pills – Take once and then repeat 1-2 weeks later. This should not be given to children aged younger than 5 years or who weigh less than 15 kg (about 35 lb), or to pregnant or lactating individuals.
The medical professional may prescribe an antibiotic if any scratched areas appear to be infected with bacteria.
After treatment, the rash and itch may take up to 4 weeks to go away while your immune system continues to react to the dead mites. However, new burrows and rashes should stop appearing 48 hours after effective treatment. If you see new burrows or papules or if the itch continues for more than 4 weeks, you may need to be treated again.
Your medical professional may also recommend steroid creams or antihistamine pills to relieve the itching. In severe cases, oral steroids may be required to decrease symptoms.
Because it may take up to 6 weeks after exposure to develop symptoms, people may be unaware that they are infested. Therefore, household members, sexual partners, and anyone else with prolonged skin-to-skin contact with a person with scabies should also be treated. Ideally, everyone should be treated at the same time to help prevent reinfestation.
Visit Urgency
See your medical professional if you develop an extremely itchy rash that does not go away. If other members of your household or close contacts have a similar itchy rash, they should also be evaluated by a medical professional.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
Centers for Disease Control and Prevention. Scabies Frequently Asked Questions (FAQs). CDC. https://www.cdc.gov/parasites/scabies/gen_info/faqs.html. Updated 2020 Sept 1.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Last modified on June 18th, 2024 at 1:57 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder













