Telangiectasia
Telangiectasias, commonly called spider veins, are dilated blood vessels in the outer layer of the skin. Telangiectasias are very common and are often caused by sun damage or aging. Although they can arise on their own in healthy people and are usually harmless, they are seen with a number of conditions, including rosacea, scleroderma, lupus, several types of inherited disorders (ataxia-telangiectasia, hereditary hemorrhagic telangiectasia, xeroderma pigmentosum, and others), or with prolonged use of oral or topical corticosteroids.
Who's At Risk?
Telangiectasias are common and can affect anyone, but they are more common in:
- Older adults.
- People who use corticosteroids for long periods.
- People with certain underlying conditions, such as rosacea, lupus, or scleroderma.
- Pregnant individuals.
- People who stand for long periods and those with varicose veins.
- People with a history of frequent sun exposure, such as people who work outdoors or who sunburn easily.
Signs & Symptoms
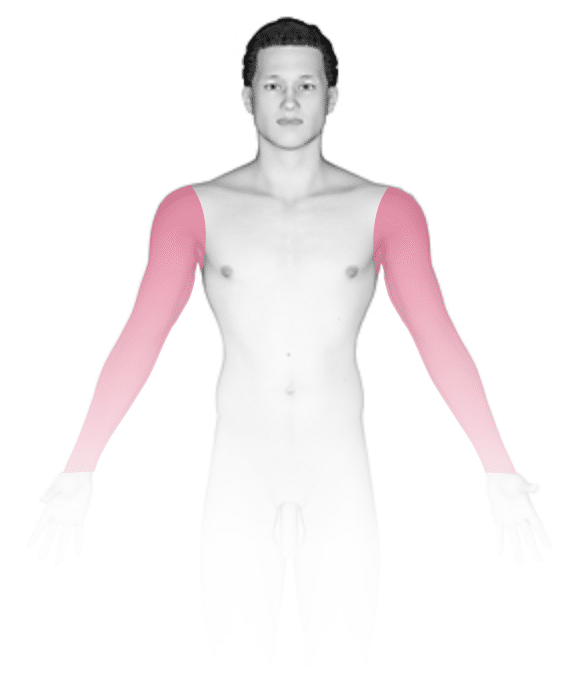
Telangiectasias can be seen anywhere on the body, but they are most common on the face (nose, cheeks, and chin) and legs (particularly the thighs, just below the knees, and the ankles).
Telangiectasias are red, blue, or purple linear marks measuring about 1 mm in width and several millimeters to centimeters in length. They disappear temporarily if you press on them with your finger (blanch).
Self-Care Guidelines
If the telangiectasias are cosmetically bothersome, you can try using cover-up makeup or self-tanning lotion to help camouflage them. Waterproof leg makeup is also available.
Treatments
If the medical professional is concerned about a potential underlying condition causing the telangiectasias, they may recommend blood tests and possibly evaluation of family members.
If there is an underlying condition causing the telangiectasias, the medical professional will help treat that condition. Your medical professional will also review your medication list to see if there may be a medication that could be contributing to telangiectasia formation.
The appearance of telangiectasias may be improved by laser treatments and burning (electrosurgery).
Laser treatment of telangiectasias on the leg is more difficult and may leave marks. Injection of chemicals to cause scarring in the blood vessel, thereby closing it (known as sclerotherapy), is often preferred for treating telangiectasias on the legs.
Visit Urgency
See your medical professional if you have a family history of similar marks, any personal or family history of bleeding from the gastrointestinal tract, lesions on the mouth or eye lining, or repeated bleeding from a lesion. If the spider veins are on your legs and you have symptomatic varicose veins, such as swollen legs, seek care.
If the telangiectasias are a cosmetic concern, you can seek medical advice for treatment.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 18th, 2024 at 3:32 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder





