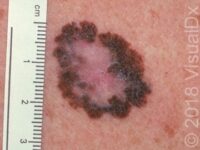
Mole (Nevus)
Nevus is the medical term for a mole. Moles (nevi) are noncancerous (benign) and can present at birth (congenital) or develop after birth (acquired). Some moles are raised and some are flat. Moles can range in color from skin-colored to pink, tan, brown, black, or even blue. Regardless of these differences, all moles are made up of collections of the pigment-producing cells of the skin (melanocytes). After moles stop growing, they may persist or they may become smaller later in life. Sun exposure and family tendency (heredity) play a role in the development of moles. Moles may sometimes become inflamed or irritated by friction from rubbing or contact with rough clothing or by other types of injury. Common acquired moles are benign and are considered normal.
Who's At Risk?
Moles may occur in people of any age, race / ethnicity, and sex, but they most commonly appear between the ages of 10 and 30 years. Individuals with lighter skin colors are more likely to develop moles.
Signs & Symptoms
- Moles may occur anywhere on the body, including the nails, palms, and soles.
- Moles may be raised or flat.
- The color of moles may vary from pink to skin-colored to brown, but they may be darker in people with darker skin colors.
- Benign moles are usually symmetrical, have smooth borders, are uniform in color, and are generally smaller than the size of a pencil eraser (6 mm).
Self-Care Guidelines
- Protective measures such as avoiding skin exposure to sunlight during peak sun hours (10 AM to 3 PM), wearing protective clothing, and applying high sun protection factor (SPF) sunscreen are essential for reducing exposure to harmful ultraviolet (UV) light.
- Monthly self-examination of the skin is helpful to detect new lesions or changes in existing lesions.
- Make sure your moles don’t have any signs of skin cancer (melanoma). Note the ABCDEs of melanoma lesions:
A – Asymmetry: One half of the lesion does not mirror the other half.
B – Border: The borders are irregular or vague (indistinct).
C – Color: More than one color may be noted within the mole.
D – Diameter: Size greater than 6 mm (roughly the size of a pencil eraser) may be concerning.
E – Evolving: Notable changes in the lesion over time are suspicious signs for skin cancer.
Treatments
Benign moles do not require treatment, although they may be surgically removed if they are cosmetically bothersome or if they become inflamed or irritated.
Visit Urgency
- The occurrence of a new mole in an adult over the age of 50 is unusual; if it occurs, see your medical professional for evaluation.
- Seek medical evaluation if you are unsure about the nature of a mole, if you note changes within a mole, or if a mole becomes irritated or painful. Additionally, seek medical evaluation if any of the ABCDEs are present.
- People with multiple moles and unusual (atypical) moles should be examined by a dermatologist every 4-12 months, depending on their personal history and family history.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 26th, 2024 at 12:00 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder



