Basal Cell Carcinoma
Basal cell carcinoma (BCC) is the most common form of skin cancer. BCCs usually occur on sun-damaged skin, especially in individuals with lighter skin colors with a long history of chronic sun exposure. Although BCC requires treatment to prevent it from spreading or becoming deeply invasive, BCCs do not typically metastasize (spread to lymph nodes or internal organs).
There are several subtypes of BCC, including:
- Superficial BCCs, which are very common and typically appear as a single small, scaly, pink, or reddish slightly raised patch (an area of skin larger than a thumbnail) with a distinct border. They tend to be slow-growing and, as the name implies, very thin. Therefore, they do not necessarily need the more aggressive forms of treatment that some other types of skin cancer require.
- Nodular BCCs, which are very common and usually appear as pink, shiny papules or nodules that occasionally bleed.
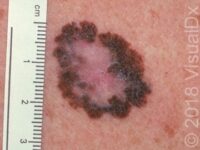
- Pigmented BCCs, which can appear as a brown, blue, gray, or black papule or nodule. It may have more than one of the colors mentioned here and also contain tiny blood vessels (telangiectasias).
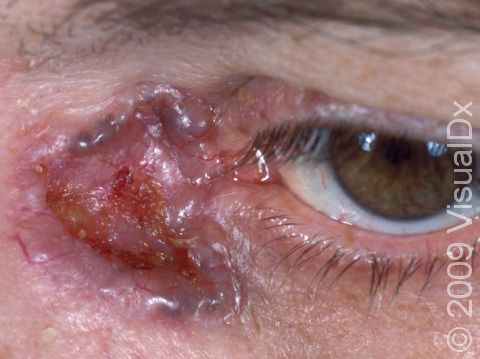
- Infiltrating BCCs, which can be more aggressive and locally destructive than other types of BCC. They can invade more deeply and widely than their appearance suggests. For this reason, it is important to treat them early.
Other common types of skin cancer include squamous cell carcinoma and melanoma.
Who's At Risk?
Although anyone of any race / ethnicity and any age can develop BCC, the overwhelming majority of people with this type of skin cancer are White and middle-aged or elderly individuals. In fact, more than 99% of people with BCC are White, and more than 95% are aged 40-80 years. Men and women seem to develop BCC fairly equally. Pigmented BCC is the most common subtype of BCC among people with darker skin colors. Pigmented BCCs are twice as common in Hispanic individuals than White individuals.
Sun exposure plays a large role in the development of BCC. People who live in sunnier climates or who spend time outdoors due to work or hobbies are more likely to have BCC.
Signs & Symptoms
The most common location for BCC is on sun-damaged skin, especially the:
- Face.
- Head, including the ears.
- Neck.
- Chest.
- Upper back.
However, BCCs can occur on any part of the skin (eg, arms, legs, and even the genitals), except for the palms and soles.
Superficial BCCs often appear as a pink or red dry, scaly patch. They slowly enlarge and may develop a raised edge. Often, people mistake a superficial BCC as a dry patch of skin or a rash that won’t go away. This subtype of BCC is most often found on the trunk (chest or upper back), arms, or legs.
Nodular BCCs are described as “pearly” in appearance, meaning they appear shiny. They are usually skin-colored or pink papules or nodules, and telangiectasias can frequently be seen on their surface. As a nodular BCC grows, it can develop a shallow depression in its center, and bleeding with minor trauma can occur. This subtype of BCC is most often seen on the face, especially the cheeks, nose, forehead, and eyelids.
Pigmented BCCs appear as brown, blue, gray, or black papules or nodules. Sometimes they will have more than one color and telangiectasias, as well as a rolled / rounded edge or a depressed center. This subtype can occur on any body location but is often found on the head and neck.
Infiltrating BCCs tend to appear as scar-like growths on the skin. They can be slightly shiny and sometimes have telangiectasias, sores (erosions), or scabs on their surface. They may be skin-colored, white, yellow, or pink. This subtype of BCC is most common on the face and scalp.
In darker skin colors, the redness may be harder to see, and there may be a brown, black, or blue color seen in the center of the spot.
Self-Care Guidelines
Preventing sun damage is crucial to avoiding the development of BCC. Wearing a broad-spectrum sunscreen with sun protection factor (SPF) 30 or higher as well as wide-brimmed hats, sunglasses, and long-sleeved shirts can help avoid some sun exposure. Some manufacturers make specialty clothing with an ultraviolet protection factor (UPF) rating. In addition, staying out of the sun when it is the strongest (between 10:00 AM and 3:00 PM) is advised.
Once a month, you should perform a self-exam to look for signs of skin cancer. It is best to perform the exam in a well-lit area after a shower or bath. Use a full-length mirror with the added assistance of a hand mirror. Using a hair dryer can help you examine any areas of skin covered by hair, such as your scalp.
- In front of a full-length mirror, inspect the front of your body, making sure to look at the front of your neck, chest (including under breasts), legs, and genital area.
- With your arms raised, inspect both sides of your body, making sure to examine your underarms and armpits.
- With your elbows bent, examine the front and back of your arms as well as your elbows, hands, fingers, the areas between your fingers, and your fingernails.
- Inspect the tops and bottoms of your feet, the areas between your toes, and your toenails.
- With your back to the mirror and holding a hand mirror, inspect the back of your body, including the back of your neck, shoulders, legs, and buttocks.
- Using a hand mirror, examine your scalp and face.
As you perform your monthly self-exam, familiarize yourself with the moles, freckles, and other marks on your body, and look for any changes in them from month to month, including changes in shape, size, color, and other changes, such as moles that bleed or itch.
Treatments
If your medical professional suspects a BCC, they will first want to establish the correct diagnosis by performing a biopsy of the lesion. The procedure involves:
- Numbing the skin with an injectable anesthetic.
- Sampling a small piece of skin.
- Having the skin sample examined under the microscope by a dermatopathologist.
The treatment depends on a variety of factors, including the subtype and size of the cancer, location on the body, and microscopic features described in the biopsy report.
Mohs surgery is considered the most effective treatment for many types of BCCs. It is particularly useful for BCCs located on the nose, ears, and lips. It is also best for BCCs that may be higher risk due to their type or size, or because they occur on a body location where BCCs are more likely to recur. In this technique, the physician takes tiny slivers of skin from the cancer site until the skin cancer is completely removed.
Other possible treatments for lower-risk BCCs include:
- Standard surgical excision.
- Physical destruction of the cancer by a process known as electrodesiccation and curettage (ED&C).
- Topical cancer therapies, such as imiquimod or 5-fluorouracil.
- Treatment with radiation or specialized light procedures.
The cure rate for most BCCs is very good, especially when diagnosed early and treated appropriately.
Visit Urgency
If you develop a new lesion on sun-exposed skin or if you have a spot that bleeds easily or does not seem to be healing, you should make an appointment with a medical professional, such as a dermatologist.
Be sure to tell them when you first noticed the lesion and what symptoms there are (such as easy bleeding or itching). Also be sure to ask your family members if they have ever been diagnosed with skin cancer, and relay this information to your medical professional.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 26th, 2024 at 12:30 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder