Drug Eruption
A drug eruption, also known as a drug rash or drug reaction, is a skin condition caused by a medication. Any medication can cause a drug eruption, and drug eruptions can range in severity from mild to severe. While they range in appearance and severity, there is most commonly a red, itchy rash of some form.
Who's At Risk?
Drug eruptions can appear on people of any age, race / ethnicity, or sex. However, women are more likely than men to develop drug eruptions, and they tend to occur more frequently in people older than 65 years.
Additional factors that predispose an individual to developing a drug eruption include:
- Having a weakened immune system due to underlying illness or medication.
- Taking more than 3 medicines daily.
Although any medication can cause a drug eruption, the most common types that trigger a drug eruption include:
- Antibiotics, such as penicillin or sulfa drugs.
- Anti-inflammatory medicines, such as ibuprofen, naproxen, or indomethacin.
- Seizure medications (anticonvulsants), such as phenytoin or carbamazepine.
- Chemotherapy agents.
- Medicines for psychiatric illnesses (psychotropic medications).
- High blood pressure medications, such as diuretics and angiotensin-converting enzyme (ACE) inhibitors.
- Medication for gout (allopurinol).
- HIV medications.
- Iodine, especially that found in x-ray contrast dye.
Signs & Symptoms
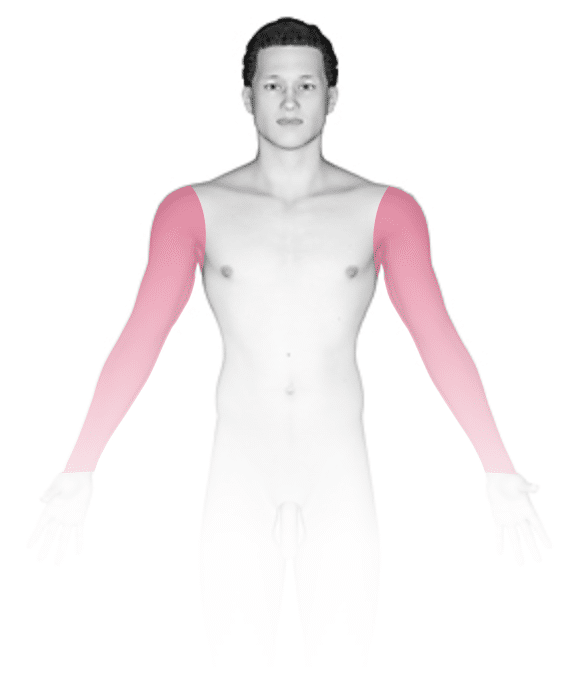
Drug eruptions can appear as a variety of skin rashes, including pink-to-red papules (small, solid bumps), urticaria (hives), vesicles (small blisters), pustules (small pus-filled bumps), bullae (blisters larger than a thumbnail), or sensitivity to sunlight. In darker skin colors, the redness may be harder to see. Drug eruptions may involve the entire skin surface, or they may be limited to one or a few body parts. Most often, the rash appears in skin fold areas such as the underarms or groin, on the trunk, or on the arms and legs.
Itching is common with many drug eruptions, and there may be a fever. If a fever is present, the skin is tender, or the membranes inside the mouth or the genitalia are involved, then a more serious skin condition may be present.
Self-Care Guidelines
For a widespread or severe drug eruption, self-care is not recommended. Call your medical professional or visit an urgent care if your symptoms are severe. If you have skin pain or mouth or genital involvement, seek care immediately at an emergency room or call 911. If you have difficulty breathing, a rapid heart rate, or your tongue, lips, throat, or face swell, seek emergency care or call 911.
For a mild drug eruption, you may try:
- Taking cool showers or applying cool compresses.
- Applying calamine lotion to the rash.
- Taking an antihistamine, such as cetirizine (eg, Zyrtec) or diphenhydramine (eg, Benadryl).
Treatments
If your medical professional suspects a drug eruption, they may want to establish the correct diagnosis by performing a biopsy of the lesion. In addition, they may want to perform blood work to look for signs of an allergic reaction.
The best treatment for a drug eruption is to stop the medication that is causing it. However, stopping a prescription medication should be done only with a medical professional’s guidance. After discontinuing a medicine, it may take 5-10 days to see an improvement in the skin and up to 3 weeks for the rash to resolve completely.
Other treatments to improve symptoms may include:
- Oral antihistamine pills, such as diphenhydramine hydrochloride, hydroxyzine, cetirizine, or loratadine, for itching.
- Topical corticosteroid (cortisone) creams or lotions for red, inflamed skin.
- Oral corticosteroids (eg, prednisone) for severe eruptions.
- Topical antibiotic ointments for open sores.
Visit Urgency
If you start a new medication and develop a rash, immediately notify the medical professional who prescribed the medicine.
Prepare a list of all your medications, including prescription and over-the-counter pills as well as topical creams, vitamins, and herbal or homeopathic remedies, for the medical professional. Be sure to include any medicines you take only occasionally. If possible, try to document when you started taking each medication. Also note any previous reactions you have had to medicines or foods.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on June 17th, 2024 at 12:57 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder


