Animal Bites, First Aid
Bites can be caused by wild animals, domestic animals, and humans, and they can range from mild to serious. It is important to assess both the severity of the bite and the risk for infection to determine the appropriate first aid and care.
Note: If the bite is from a wild animal or from a domestic animal whose immunization status is unknown, rabies is a concern. Seek prompt care from a medical professional, even if the bite is mild and the skin appears to be barely broken. Immediate vaccination can prevent rabies from developing. While rabies in humans is rare, it does occur and is typically fatal.
Rabies is more common in raccoons, skunks, bats, and foxes than in domestic cats and dogs; it can occur but is rare in wild or domestic rodents, such as rabbits, squirrels, and mice.
If you have been bitten by an animal and its rabies vaccination status is unknown, notify police or animal control. DO NOT attempt to capture a potentially rabid animal yourself. Be ready to tell officials what the animal looks like and where it is likely located so they can capture it and determine next steps.
Who's At Risk?
Animal bites are common and occur most frequently in children. Most animal bites come from domestic dogs. Cat bites are less common, but the risk of infection from a cat bite is higher than that from a dog bite.
Incidence of wild animal bites varies by region.
Signs & Symptoms
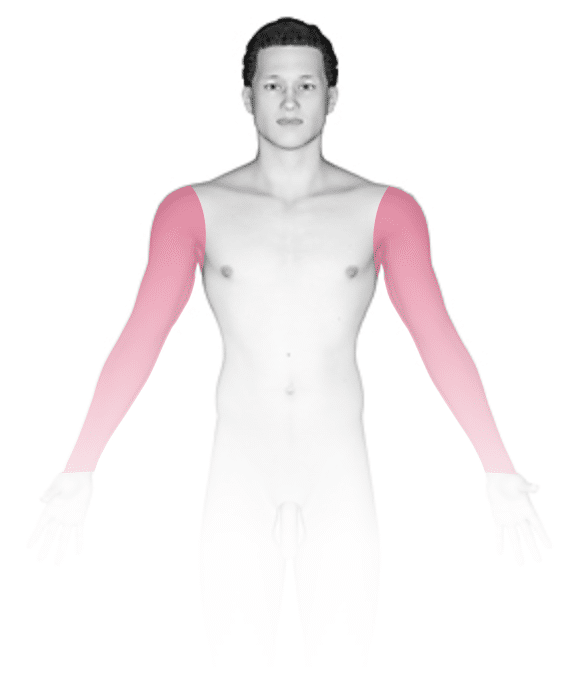
Most bites occur on the fingers of the dominant hand. Children are also prone to bites on the head and neck.
The wound is typically a puncture wound with visible teeth marks, possibly quite deep in the skin and muscle.
Self-Care Guidelines
First aid for minor bite wounds:
Minor bite wounds are wounds where the skin is only slightly broken; bites from a human (eg, a child); and bites from a domestic animal vaccinated against rabies.
- Thoroughly wash the wound with soapy water.
- Apply a topical antibiotic ointment, such as one containing bacitracin (eg, Neosporin, Polysporin), to the affected area.
- Cover the wound with a clean bandage.
- Watch for signs of infection (eg, the affected area is very red or warm to the touch, painful, oozing pus, or blood-filled).
- If the bite is on the hand or finger, call your medical professional, as antibiotics are often needed.
First aid for severe bite wounds:
Severe bite wounds are wounds that are torn, deep (including deep punctures), or bleeding badly.
- Attempt to stop the bleeding by applying pressure to the affected area with a clean, dry cloth.
- For further care, seek prompt medical assistance.
Treatments
The medical professional may give a tetanus vaccine for any bite if previous tetanus vaccination was more than 5 years ago. If infection occurs at the bite site, the medical professional will prescribe antibiotics.
There is no cure for rabies once symptoms have developed. However, if you are promptly vaccinated against rabies after being exposed to the disease, you can develop immunity to it before symptoms develop. A medical professional will determine if rabies vaccination is needed.
Visit Urgency
Any time you have been bitten by an animal, even if it broke the skin only slightly, it is important to consider the potential for rabies. If the animal is wild or is domestic and the immunization status is unknown, seek prompt medical attention.
In the case of any animal bite, seek medical care if there are signs of infection (eg, the affected area is very red or warm to the touch, painful, oozing pus, or blood-filled).
Last modified on August 8th, 2024 at 12:43 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder

