Herpes Simplex Virus (HSV)
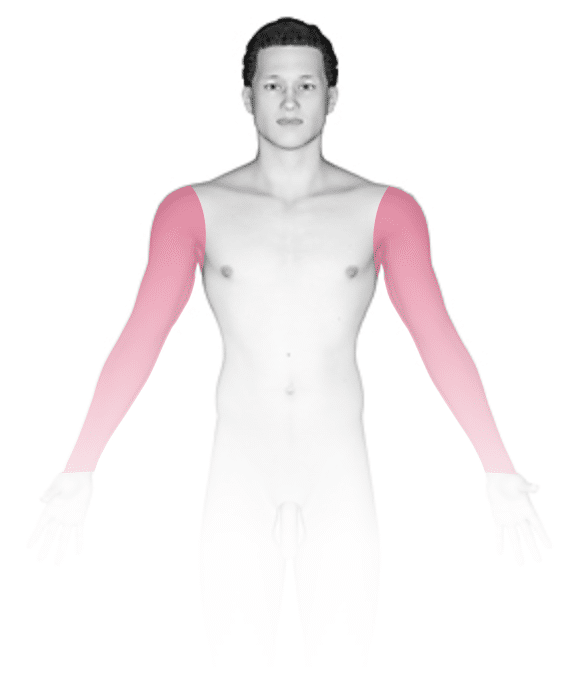
Herpes infections are caused by both herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). HSV-1 more commonly causes sores in and around the mouth. HSV-2 more commonly causes genital and anal sores. Both types of infections can appear anywhere on the body. Primary herpes is defined as the first outbreak of lesions and is usually more severe than recurrent episodes.
Herpes simplex virus (HSV) is highly contagious and is easily transmitted through direct contact with the lesions of an infected person. However, the virus can also spread in the absence of symptoms or visible lesions. Affected individuals carry the virus in their bodies for the rest of their lives.
In newborns (babies in the first month of life), HSV infection, known as neonatal herpes, can potentially be life-threatening, and symptoms almost always accompany infection. The virus is able to enter the brain and spinal fluid and can cause seizures and even death.
Who's At Risk?
HSV infections in newborns are usually the result of the virus being passed from mother to baby during childbirth. The highest risk of passing herpes to a newborn occurs when a pregnant individual develops primary herpes during the third trimester of pregnancy. In contrast, the risk of transmitting herpes to a newborn is much less (about 3%) in those who have recurrent herpes during their pregnancy. Vaginal delivery also increases the risk of transmission if active lesions are present in the genital area at the time of delivery. Neonatal herpes (within the first month of life) can be very severe, affecting the brain and other internal organs. Even with treatment, newborns have a very high risk of death.
Infants can also become infected with HSV through direct skin-to-skin contact with someone who has an active lesion. For instance:
- Kissing a child when you have an active lesion.
- Changing a diaper when there is a lesion on your hand.
- Breastfeeding with a lesion on the breast.
These infections are far less severe in nature and usually result in only sores on the mouth, lips, or other area of skin of the infant.
Signs & Symptoms
For infections right after birth, small fluid-filled bumps (vesicles) are seen on the scalp, Vesicles can be quite few, scattered, or widespread.
Most commonly, primary herpes in infants involves painful blisters and erosions of the gums and the skin around or lining the mouth. There may also be fever, swollen lymph nodes in the neck, irritability, and a poor appetite. If HSV is introduced on another body site, there may be painful blisters and sores in that location (eg, the finger, face, genitals), with swelling and similar symptoms affecting the entire body, such as fever and swollen lymph nodes.
Self-Care Guidelines
Herpes that is acquired at birth requires care in the hospital and may require intensive care unit care.
For primary herpes in infants, the goal of treatment is to make your child as comfortable as possible. They may have difficulty eating, drinking, and sleeping if they are in pain.
- Encourage your child to drink as much fluid (milk, water, or juice) as possible to avoid dehydration.
- You can give over-the-counter acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) for pain.
- Avoid contact with other children (especially newborns or those with eczema or a weak immune system) until the sores are healed.
Treatments
For herpes infections in newborns, intravenous antiviral treatment with acyclovir (Zovirax) is given along with supportive care.
For primary HSV acquired in infancy, your child’s medical professional may prescribe an antiviral medication to speed recovery of the sores. Acyclovir (Zovirax) is the only antiviral medication that is available as a liquid and that is approved for use in infants. If your child is unable to eat or drink because of mouth sores, they are at risk of becoming dehydrated. If this occurs, they may need IV (intravenous) fluids.
Visit Urgency
See your pediatrician or other medical professional if you think your baby has primary herpes and for any skin condition that is present immediately after birth.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on June 14th, 2024 at 9:45 am
Not sure what to look for?
Try our new Rash and Skin Condition Finder





