Kerion
Kerion is a condition that is caused by an inflammatory reaction to a fungal infection on the scalp (commonly known as scalp ringworm and also known as tinea capitis). A kerion appears as an inflamed, thickened, pus-filled area, and it may be accompanied by fever and swollen lymph nodes in the neck. If untreated, the kerion can lead to permanent hair loss (alopecia).
Who's At Risk?
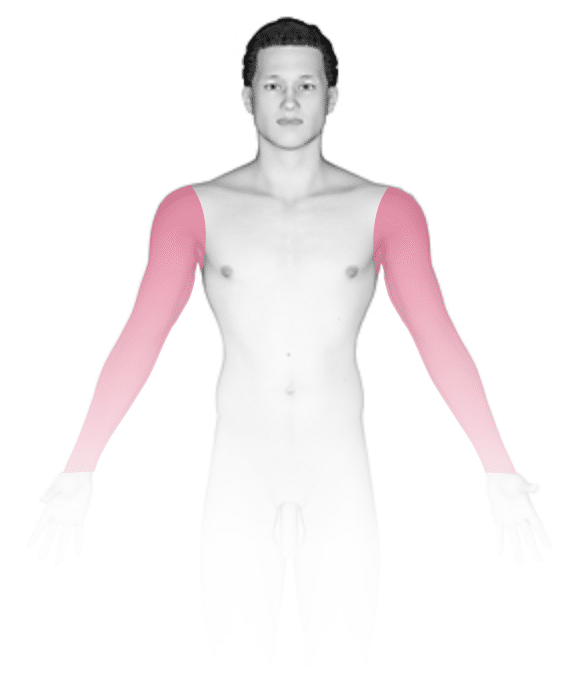
A kerion may occur in people of all races / ethnicities and sexes. However, kerions are seen almost exclusively in children. On rare occasions, kerions may be seen in teens and young adults, though. They are more common in males and in people with short hair. Other people at increased risk of developing a kerion include those:
- With a lower immune system.
- With diabetes.
- With anemia.
- With cancer.
- Who have had an organ transplant.
Signs & Symptoms
A kerion appears as a thick, “boggy” or “mushy” nodule (a solid, raised bump that is firm to the touch) or plaque (a raised or bumpy area larger than a thumbnail) on the skin, often the scalp. Its surface commonly has several pustules (pus-filled bumps) on it. The pustules can break open and drain pus.
Fever and pain may accompany the kerion. In addition, the lymph nodes at the back of the scalp, behind the ears, or along the sides of the neck may be swollen.
Self-Care Guidelines
There are no effective self-care measures to treat a kerion. If you suspect your child may have a kerion, it is important that they get treatment to avoid potential permanent hair loss.
Note that people with a fungal infection should avoid sharing items such as bedding, towels, and hairbrushes.
Treatments
Medical professionals can often diagnose a kerion just by visually inspecting it. However, to confirm the diagnosis, they may want to scrape some surface skin scales onto a slide and examine them under a microscope. This procedure, called a KOH (potassium hydroxide) preparation, allows the medical professional to look for signs of a fungal infection.
Sometimes the medical professional will also perform a fungal culture to determine what exact type of fungus is causing the infection or to see if there is a bacterial infection in addition to the fungal infection.
Tinea and kerions can be treated with oral antifungal medicines. Both usually require at least 6-8 weeks of treatment with oral antifungal pills or syrup, including:
- Griseofulvin.
- Terbinafine.
- Itraconazole.
- Fluconazole.
Often, the medical professional will also prescribe a medicated shampoo to reduce the risk of spreading the infection to others, such as:
- Selenium sulfide shampoo.
- Ketoconazole shampoo.
If the child also has a bacterial infection, the medical professional may prescribe an oral antibiotic as well.
If the kerion is particularly tender or painful, your child’s medical professional may recommend starting oral corticosteroids (cortisone pills or syrup). Steroids are strong medications that can quickly reduce the inflammation present in the kerion.
Visit Urgency
See your child’s medical professional for evaluation if the child is losing hair or if they have an itchy, scaly spot or spots on the scalp or elsewhere on the body. If your child develops a thick, pus-filled bump on the scalp or other area of the body, it is important to see their medical professional to determine if there is a kerion or some other infection that requires treatment.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on June 17th, 2024 at 3:55 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder





