Pubic Lice (Pediculosis Pubis)
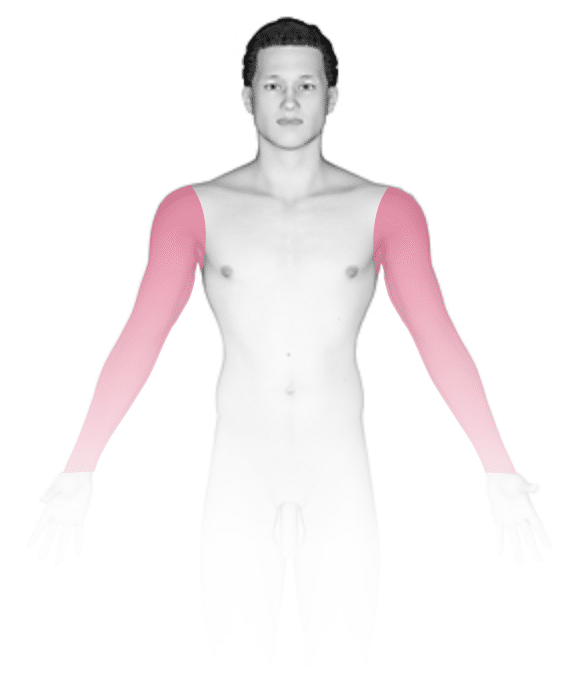
Pubic lice, also known as crab lice or crabs, are wingless, bloodsucking insects that can live and multiply on coarse hair, especially pubic hair. Hair in the armpits, eyelashes, eyebrows, or scalp can sometimes be affected, as well. Pubic lice infestation (pediculosis pubis) usually causes itching. It is spread by close physical contact or contaminated personal items such as clothing, bedding, or towels. Pubic lice infestations may occur with other sexually transmitted infections (STIs).
Who's At Risk?
Pubic lice can affect all races / ethnicities in all levels of society. Men are more commonly affected by public lice, possibly because they have more coarse body hair.
Pubic lice is most frequent in people aged of 15-40 years who are sexually active.
Signs & Symptoms
Lice and their eggs (nits) can be seen attached to the hair in the pubic region and other areas where there is coarse hair. Small red or blue-gray macules (smooth, flat areas) or papules (smooth, raised areas) may be seen at the bite sites. The affected areas can be extremely itchy. Small specks of dried blood may be seen on clothing in the affected area, such as on underwear. The lymph nodes in the groin may be swollen.
Self-Care Guidelines
Avoid intimate contact with partners and avoid sharing personal items with others if you have pubic lice. Note that condoms do not prevent the transmission of pubic lice. If you are diagnosed with pubic lice, sexual partners within the prior 1-3 months should be notified and treated as well.
Additionally:
- Launder in hot water any clothing, linens, and towels that have come in contact with the infected person in the past 3 days.
- Seal potentially contaminated nonwashable objects in plastic bags for 2 weeks. (The lice will die within 2 days, and the nits will hatch and die within 2 weeks.)
- Avoid scratching the skin, as scratching can cause a secondary bacterial infection.
Treatments
Your medical professional may:
- Recommend over-the-counter or prescription treatments, such as:
- Permethrin cream rinse or pyrethrins with piperonyl butoxide.
- Malathion lotion or ivermectin lotion or oral medication.
- Advise treating any sex partners you have had within the previous 1-3 months.
Your medical professional should prescribe treatment for all infested hair-bearing areas to prevent the infestation from coming back. Eyelash involvement should not be treated with the above medications; an ophthalmic ointment or petroleum jelly (eg, Vaseline) should be used instead.
Note that you should avoid sexual contact until you and your partner(s) have been treated and reevaluated to ensure the infestation is no longer present.
Visit Urgency
See your medical professional for evaluation if you think you have pubic lice. Your medical professional can suggest the ideal treatment for your situation and advise testing for other STIs.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 14th, 2024 at 3:38 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder




