
Psoriatic Arthritis
Up to 30% of people who have plaque psoriasis develop joint inflammation (arthritis) called psoriatic arthritis. Most people develop psoriasis before developing psoriatic arthritis. However, symptoms of arthritis can appear before psoriasis in about 15% of patients or simultaneously with the development of the first skin lesions. Psoriatic arthritis presents as joint pain, stiffness, and swelling. Psoriatic arthritis commonly develops between the ages of 30 and 50, but it may occur at any age.
Who's At Risk?
Risk factors for psoriatic arthritis include a history of psoriasis and a family history of psoriatic arthritis. Individuals with plaque psoriasis involving the scalp or nails are at increased risk for psoriatic arthritis.
Signs & Symptoms
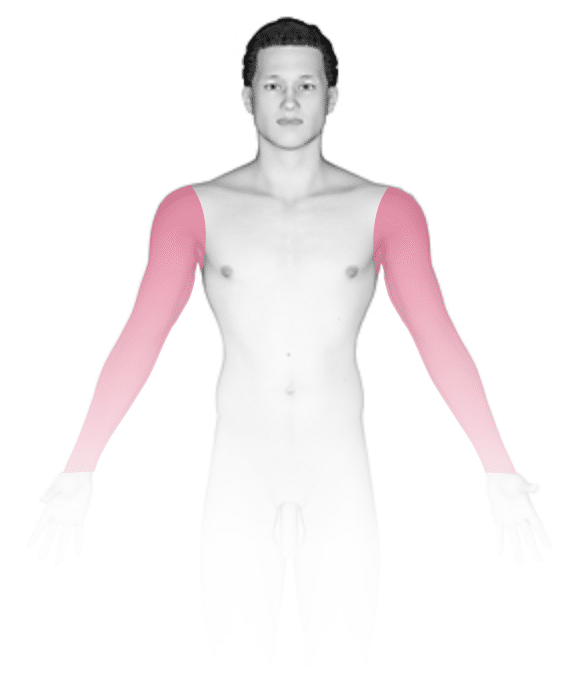
The symptoms of psoriatic arthritis tend to get worse as time goes on. It can cause joints on one or both sides of the body to become painful, with swelling and redness. In darker skin colors, the redness may be harder to see. The symptoms are similar to those of rheumatoid arthritis, but individuals with psoriatic arthritis are more likely to experience swollen fingers and toes (known as dactylitis), foot pain, and lower back pain.
Other signs and symptoms of psoriatic arthritis include:
- Pain and stiffness that is worse following long periods of inactivity, such as when getting up in the morning. Pain in the morning typically lasts longer than 1 hour and may improve over time as the joints are used throughout the day.
- Swelling of tendons (tendonitis, tenosynovitis).
- Joints that appear red or darker than the surrounding skin color and are warm, tender, and painful.
- Fingers that appear swollen (dactylitis).
- Nails that appear to pull away or separate from the nail bed (onycholysis) or that have small indents called pits.
Some with psoriatic arthritis also develop eye symptoms, including dry eyes, irritation (uveitis), foreign body sensation, and redness in the whites of the eyes.
Self-Care Guidelines
To help ease the symptoms of psoriatic arthritis:
- Maintain a healthy weight, such as by eating a plant-based diet (whole grains, fruits, and vegetables).
- Exercise regularly, particularly with activities that do not stress your joints (swimming, walking, and bicycling).
- Avoid straining your joints.
- Use hot and cold therapy to reduce swelling and pain.
- Use over-the-counter pain relievers such as ibuprofen (Advil, Motrin) or naproxen sodium (Aleve).
- Participate in stress-management techniques and support groups. Ask your healthcare provider or contact the National Psoriasis Foundation at https://www.psoriasis.org/about-psoriatic-arthritis.
Patient Support Resources
The National Psoriasis Foundation is a useful resource for patients and health professionals that has additional information regarding psoriasis and the various available treatments. The National Psoriasis Foundation website includes access to psoriasis-related articles, psoriasis research, a directory of health care professionals with an expertise in psoriasis, and opportunities for patients to volunteer or get involved in upcoming events.
Treatments
You may be referred to both a dermatologist and a rheumatologist to control inflammation, pain, and discomfort. It is important to seek medical treatment for psoriatic arthritis because long-standing untreated disease may cause irreversible joint tissue damage and/or bone loss.
Your dermatologist or rheumatologist may recommend and prescribe a range of treatments to reduce symptoms:
- Steroid injections can quickly reduce inflammation. However, oral steroids should be used with caution because they may cause severe flares of psoriasis as the steroids wear off.
- Prescription-strength pain relievers can help, although there are side effects (stomach, liver, and kidney irritation).
- Apremilast (Otezla) is an oral medication that is approved for the treatment of psoriasis and psoriatic arthritis.
- Medications called biologics treat psoriasis and psoriatic arthritis by blocking certain actions of the immune system. They are injected under the skin (subcutaneously) or may be given intravenously. This class of medications is highly effective at treating psoriasis but may be costly if not covered by insurance. The number of injections each month and the side effects differ for each medication and should be discussed with your medical professional. These medications include:
- TNF-alpha inhibitors (eg, etanercept [Enbrel], infliximab [eg, Remicade])
- IL12/23 inhibitor (eg, ustekinumab [Stelara])
- IL-23 inhibitors (eg, guselkumab [Tremfya], risankizumab [Skyrizi])
- IL-17 inhibitors (eg, secukinumab [Cosentyx], ixekizumab [Taltz])
- Janus kinase (JAK) inhibitors (eg, tofacitinib) [Xeljanz], upadacitinib [Rinvoq]) are another newer type of medication for psoriatic arthritis.
- Methotrexate (Trexall) is a pill taken weekly that can slow the progression of arthritis. If you take this medication, you will need to see a medical professional regularly to monitor for possible side effects, such as liver damage.
If a joint is irreversibly damaged, it may be replaced with an artificial joint (by an orthopedic surgeon).
Visit Urgency
Contact your health professional if you have psoriasis and begin to develop joint pain.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on July 3rd, 2024 at 11:46 am
Not sure what to look for?
Try our new Rash and Skin Condition Finder




