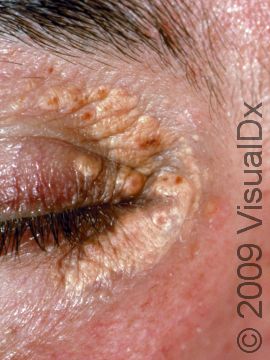
Xanthelasma Palpebrarum
Xanthelasma is a skin condition in which flat, yellow growths develop under the skin. When xanthelasma occurs on the eyelids, it is called xanthelasma palpebrarum.
Xanthelasma is often seen in people with high cholesterol or other fat (lipid) levels in the blood, and the lesions contain deposits that are lipid-rich.
Who's At Risk?
Xanthelasma can occur in people of any race / ethnicity. Females seem to be more frequently affected than males. Most individuals who develop the condition are adults, and it is rare for children and teenagers to develop xanthelasma.
Approximately half of people with xanthelasma have high amounts of lipids in their blood, such as high cholesterol or high triglycerides.
Signs & Symptoms
The most common locations for xanthelasma palpebrarum include:
- One or both upper eyelids, especially near the nose.
- One or both lower eyelids.
Xanthelasma appears as a yellow-to-orange macule (a flat, smooth area of skin), papule (a small, solid bump), or plaque (a raised area of skin larger than a thumbnail). Xanthelasma lesions range in size from 2-30 mm. They usually have a flat surface with distinct borders. Once present, xanthelasma lesions do not usually go away on their own. In fact, they frequently grow larger and more numerous.
Xanthelasma lesions are usually not itchy or tender.
Self-Care Guidelines
There are no self-care measures for xanthelasma. See your medical professional for any new skin growth to help determine the correct diagnosis.
Treatments
The medical professional can sometimes diagnose xanthelasma based on its appearance but may want to do a biopsy to confirm the diagnosis.
Once the diagnosis of xanthelasma is confirmed, your medical professional will likely check the cholesterol levels in your blood with a lipid panel. If you have a lipid abnormality, exercise and dietary modifications will likely be recommended. Many people also require oral medication to lower their lipids. Treatment of the underlying lipid abnormality does not always cure xanthelasma.
If the xanthelasma does not go away with lipid-lowering therapies and you would like them removed for cosmetic purposes, the medical professional may remove them with:
- Application of a specially formulated trichloracetic acid solution.
- Surgical removal.
- Laser treatment or use of radiofrequency.
- Freezing with liquid nitrogen (cryotherapy).
Visit Urgency
See a medical professional such as a dermatologist if any new growth develops on your skin.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 20th, 2024 at 7:03 am

Not sure what to look for?
Try our new Rash and Skin Condition Finder