Genital Herpes
Herpes simplex infection of the genitals, or genital herpes, is a common recurrent skin condition associated with infection by the herpes simplex virus (HSV). HSV infection usually appears as a group of small vesicles (fluid-filled blisters), erosions (sore areas of missing skin), or crusts (scabs) around the mouth, nose, genitals, buttocks, and lower back, although infections can develop almost anywhere on the skin. These sores can come back periodically in the same sites, called recurrent infections.
Infections with HSV are very contagious and are spread by direct contact with the skin lesions. There are 2 types of HSV: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). HSV-1 is the most common cause of infections around the mouth, lips, nose, and face, although HSV-2 can also be a cause, and HSV-2 more commonly causes lesions on the genitals and buttocks (sometimes called sacral herpes).
Both types of HSV produce 2 kinds of infections: primary and recurrent. HSV causes a primary infection in most people who are exposed to the virus. Appearing 5-7 days after a person’s first exposure to HSV, the sores of a primary infection last about 2-4 weeks. These sores heal completely, rarely leaving a scar. Affected individuals carry the virus in their bodies for the rest of their lives.
Certain triggers can cause the hibernating (latent) virus to wake up, become active, and travel back to the skin. These recurrent HSV infections may develop frequently (every few weeks), or they may never develop. Recurrent infections tend to be milder than primary infections and generally occur in the same location as the primary infection.
Who's At Risk?
HSV infections occur in people of all races / ethnicities, ages, and sexes. Genital herpes can affect anyone who is sexually active.
Herpes is spread from person to person by direct skin-to-skin contact. The virus is most contagious when there are visible sores in the genital region. HSV can also be spread when there are no sores present, however, which is called asymptomatic shedding. Only about 20% of people who are infected with HSV develop visible blisters or sores, which means most people with HSV have not been diagnosed and are unaware of their condition. This means they can unknowingly transmit the infection to their sexual partners.
Signs & Symptoms
Shortly after exposure to the virus, a newly infected person may develop vesicles or pustules (pus-filled bumps), occurring singly or in a group. These vesicles and pustules are usually quite fragile, so people may never notice them but instead see tiny erosions (open sores). These painful erosions subsequently become scabbed over. The scabs eventually fall off, leaving a red or hyperpigmented (darker) area that finally fades. The primary outbreak typically lasts 2-4 weeks.
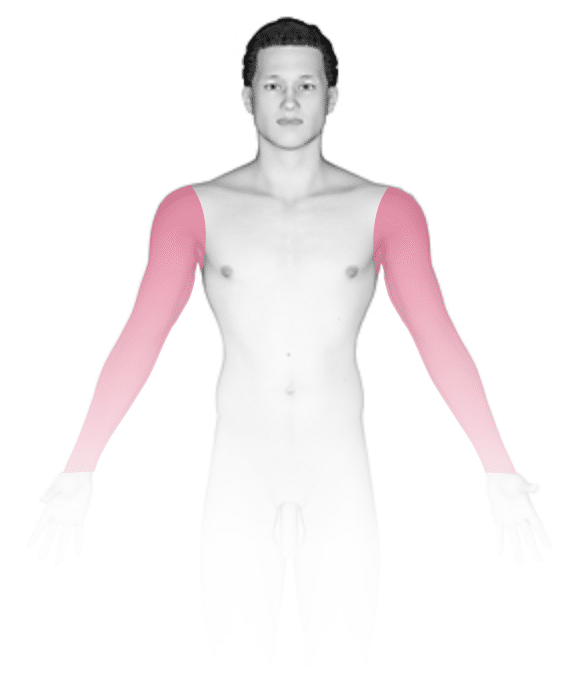
In women, the most common locations for genital herpes infection are the external genitalia, vagina, cervix, buttocks, and anus. In men, the most common locations are the penis, scrotum, upper thighs, buttocks, and anus.
Primary genital HSV infection can be severe, with many painful blisters causing pain and burning with urination and vaginal or urethral discharge. People may also develop fever, headaches, muscle aches, and fatigue with a primary outbreak.
Recurrent HSV infections are usually milder than the primary infection, but the lesions look similar. Many people with recurrent HSV infections have burning, tingling, or pain in the area of the outbreak up to 24 hours before any visible signs. This is called the prodromal phase of the infection.
Most people will have a recurrence of genital herpes during the first year after a primary infection. Note, however, that some people never develop the symptoms of a primary HSV infection and may mistake a recurrent infection for a primary infection. On average, most people will get about 4 outbreaks per year, although the frequency of recurrence is variable and tends to decrease over the years.
A recurrence of genital herpes usually occurs spontaneously, but it can also be triggered by:
- Fever or illness.
- Sun exposure.
- Hormonal changes, such as those due to menstruation or pregnancy.
- Stress.
- Trauma (eg, a cut).
- Surgery.
- Immunosuppression.
- Friction to the area (eg, with sexual intercourse or tight-fitting clothes).
Self-Care Guidelines
Acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) may help reduce pain, fever, and muscle aches that accompany the herpes sores. Applying ice packs or baking soda compresses to the affected areas may relieve some of the swelling and discomfort. Wear loose-fitting clothes and cotton underwear, and keep the infected area clean and dry.
Because HSV infections are very contagious, it is important to take the following steps to prevent spread of the virus during the prodromal phase (burning, tingling, or pain) and active phase (presence of blisters or sores) of genital HSV infections:
- Avoid sharing towels and other personal care items.
- Wash your hands with soap and water if you touch an active lesion. HSV can be spread to other parts of your body via infected hands.
- Avoid sexual contact (including oral, vaginal, and anal sex) during both the prodromal phase and the active phase.
Unfortunately, the virus can still be spread even when someone does not have lesions. Therefore, condoms should be used between outbreaks, even if no sores are present. Note, though, that while using condoms lowers the risk of spreading herpes, there is still risk of transmission.
Treatments
Most HSV infections are easy for medical professionals to diagnose. On occasion, however, a swab from the infected skin may be sent to the laboratory to confirm the diagnosis. A blood test can also be performed to determine if you have been exposed to the virus. Your medical professional may recommend a blood test for your partner to determine if they have been exposed to herpes in the past or if they are at risk for contracting the virus.
Untreated HSV outbreaks will go away on their own, but antiviral medications can reduce symptoms, shorten their duration, and decrease the chance of spreading the virus. These medicines are most effective if taken during the first 24 hours of symptoms. If you experience burning and tingling before the appearance of blisters, you can start antiviral medications as soon as you start feeling the symptoms. Unfortunately, these medicines do not cure HSV infections.
Treatment for primary and recurrent HSV infections are oral antiviral medications such as acyclovir (Zovirax), valacyclovir (Valtrex), and famciclovir (Famvir). Talk to your medical professional about getting a prescription for these medicines for possible future outbreaks, as they are most effective if taken early.
If you have frequent or severe herpes outbreaks, your medical professional may recommend taking an antiviral medication every day, called suppressive therapy, to decrease the frequency and severity of outbreaks. This type of therapy may also be effective in decreasing the chance that an uninfected partner will acquire the virus. If you are taking a daily antiviral medicine to suppress your outbreaks, talk to your medical professional yearly about potentially stopping these medicines or seeing if you still need daily treatment.
Visit Urgency
If you develop new painful sores in or around the genitals, see a medical professional as soon as possible because HSV treatment is much more effective if started early.
Recurrent outbreaks of genital HSV usually do not require medical care. However, because some people have milder forms of herpes, see a medical professional for any recurring rash in the genital area, even if you think it is just from bug bites, jock itch, or any other condition.
If you have an underlying medical condition such as cancer or HIV, if you have undergone organ transplantation, or if you are pregnant, you are at higher risk for more serious complications from genital herpes. Seek medical advice as soon as possible if you develop any lesions.
Genital herpes can also be passed to a newborn baby during delivery through contact with a lesion in the genital tract. Be sure to speak with your obstetrician or other medical professional about the possible risk to your baby if you have genital herpes.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 26th, 2024 at 11:22 am
Not sure what to look for?
Try our new Rash and Skin Condition Finder









