Nipple Dermatitis
Nipple dermatitis is inflammation that leads to scaling, cracking, redness, itchiness, or soreness of either one or both nipples. There are several possible causes of nipple dermatitis, including:
- Eczema (atopic dermatitis).
- An allergic reaction (allergic contact dermatitis) or local irritation (irritant contact dermatitis), such as from soaps, detergents, or chlorine.
Nipple dermatitis in breastfeeding individuals may become superinfected with yeast.
A rare form of breast cancer, Paget disease, may mimic nipple dermatitis. This may occur in men and women and is usually seen on one breast in adults aged 50 and older.
Who's At Risk?
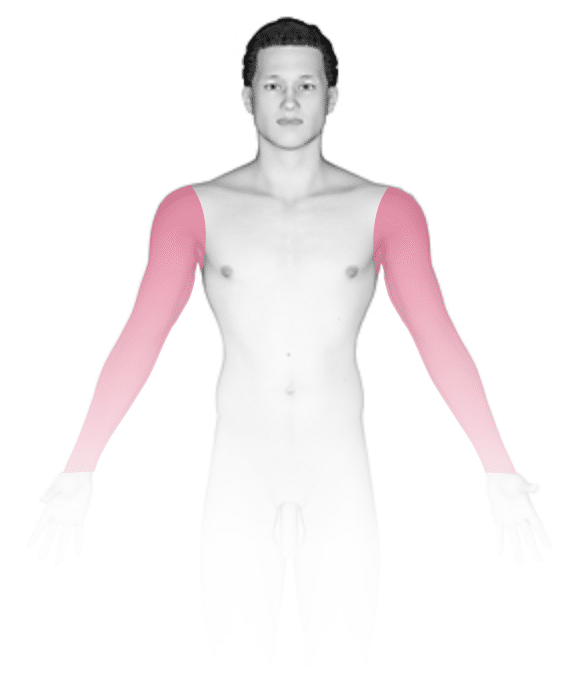
Nipple dermatitis can occur in women and men. It is common in individuals with a history of eczema (atopic dermatitis) or easily irritated skin. Irritation from clothing or friction during exercise, such as running, is another common cause.
Nipple dermatitis is also common in individuals who breastfeed. Allergic reactions may occur from either food particles in a nursing infant’s mouth or from lotions or creams applied to the nipple area. Individuals who breastfeed that have a history of vaginal yeast infection (vulvovaginal candidiasis) or whose infants also use a bottle or pacifier may be at higher risk for a yeast nipple infection.
Signs & Symptoms
Both the nipple itself and the surrounding area (the areola) may be scaly and red or darker than the surrounding skin. The area may ooze or crust, and it may be cracked, itchy, or tender.
Self-Care Guidelines
- Avoid washing the area with soap; wash with just water.
- Wash clothing with a mild laundry detergent (eg, All Free and Clear), and double rinse to remove any irritating soap residue.
- Acetaminophen (eg, Tylenol) or ibuprofen (eg, Advil, Motrin) can be taken for associated pain.
- Apply 0.5% or 1% hydrocortisone ointment (available over the counter) twice daily to the irritated area, and protect the area from friction from clothing.
- If the area feels uncomfortable, apply a warm water compress and then apply petroleum jelly (eg, Vaseline) or an ointment (eg, Aquaphor) in a thin layer. Stop use of any other creams or lotions on the skin area.
- Either wear no bra or wear a cotton bra and wash it with fragrance-free soap. Bras with few or no seams are best.
Additionally, individuals who are breastfeeding should:
- Cleanse the area after breastfeeding with a soft warm-water-moistened cloth, and then apply either purified lanolin (eg, Lansinoh HPA Lanolin) or petroleum jelly (eg, Vaseline). Do not wash off before breastfeeding again.
- Get help from a breastfeeding counselor if there are problems with the baby positioning or latching on to the breast properly.
The following practices are not recommended:
- The use of warmed tea bags on the nipples
- Drying the breast with a hairdryer
- The use of topical agents such as Bag Balm
- The use of nipple shields
Treatments
The medical professional may:
- Prescribe a topical corticosteroid.
- Prescribe a topical antifungal cream if there are signs of a yeast infection. The baby will also be treated if you are breastfeeding.
- Prescribe oral antibiotics if there is an associated bacterial infection.
- Perform a skin biopsy to rule out Paget disease.
Visit Urgency
If there is no improvement in a few days with self-care measures, seek medical help. Be sure to seek help if there is fever or spreading redness and pain of the breast.
Individuals who are breastfeeding should seek care if the baby has signs of thrush (oral candidiasis), for example white patches in the mouth, such as on the tongue.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 17th, 2024 at 11:49 am
Not sure what to look for?
Try our new Rash and Skin Condition Finder



