Scalp Ringworm (Tinea Capitis)
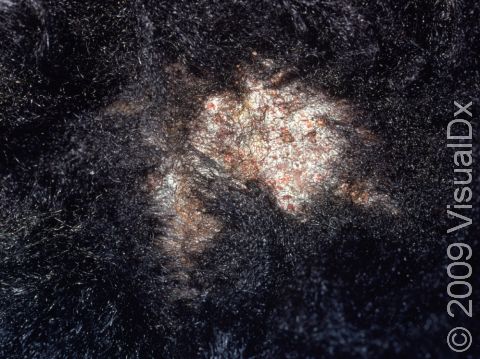
Tinea capitis, commonly known as scalp ringworm, is a fungal infection of the scalp and hair that appears as scaly plaques (raised areas of skin larger than a thumbnail) of broken hair on the head.
Scalp ringworm may be spread by direct contact with infected people or with contaminated objects (such as combs, pillows, and sofas). Less commonly, the fungus may be spread from infected animals (especially cats or dogs) or from the soil.
Who's At Risk?
Scalp ringworm may occur in people of any age, race / ethnicity, or sex. However, it is most frequently seen in children, especially those aged 3-7 years.
Signs & Symptoms
Scalp ringworm appears as one or more round or oval plaques covered with gray sheets of scale and is often accompanied by hair loss (alopecia) in the area. In lighter skin colors, the border can be pink or red, whereas in darker skin colors, it can be dark red, purple, brown, or grayish. The area may be inflamed, and small pustules (pus-filled bumps) may appear. There may be tiny black dots that appear on the surface of the scalp from broken hairs.
Although the scalp is the most common location for this type of ringworm, the eyebrows and eyelash areas can also occasionally be affected.
Lymph nodes at the back of the scalp, behind the ears, or along the sides of the neck may be swollen. Scalp ringworm is usually itchy.
One complication of scalp ringworm is a kerion, which is a thick, “boggy” or “mushy” nodule (a solid, raised bump that is firm to the touch) or plaque (a raised or bumpy area larger than a thumbnail) on the skin. If not treated aggressively, a kerion can lead to scarring and permanent hair loss.
Self-Care Guidelines
There are no effective self-care measures to treat scalp ringworm.
To prevent scalp ringworm:
- Have your child avoid close contact with infected people and pets.
- Have your child avoid sharing combs, brushes, hats, and hair accessories with friends and household members.
If your child has scalp ringworm, they should not share towels, clothing, or other personal items with others until the lesions have cleared. Also evaluate other family members for ringworm.
Treatments
To confirm the diagnosis of scalp ringworm, the medical professional may scrape some scales onto a slide and examine them under a microscope. This procedure, called a KOH (potassium hydroxide) preparation, allows the medical professional to look for signs of fungal infection.
Sometimes the medical professional will also perform a skin culture to document the presence of fungus or to discover the particular fungus that is causing the scalp ringworm.
Scalp ringworm is treated with oral antifungal medicines because the fungus invades deep into the hair follicle, where topical creams and lotions cannot penetrate. Scalp ringworm usually requires at least 6-8 weeks of treatment with oral antifungal pills or syrup, including:
- Griseofulvin.
- Terbinafine.
- Itraconazole.
- Fluconazole.
The medical professional may also prescribe a medicated shampoo to reduce the risk of spreading the scalp ringworm to someone else, such as:
- Selenium sulfide shampoo.
- Ketoconazole shampoo.
Visit Urgency
See your child’s medical professional if they have hair loss or itchy, scaly plaques on the scalp, especially if the affected areas are deep and tender or if the child has a fever or swollen lymph glands.
If a close contact of your child (eg, a sibling or classmate) is diagnosed with scalp ringworm, make sure you examine your child’s scalp by looking for scaly spots. If you are suspicious about an area, take the child to see a medical professional for an examination.
If your child is diagnosed with scalp ringworm, have any household pets evaluated by a veterinarian to make sure that they do not also have a fungal infection. If the veterinarian discovers an infection, be sure to have the animal treated.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on June 17th, 2024 at 4:30 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder