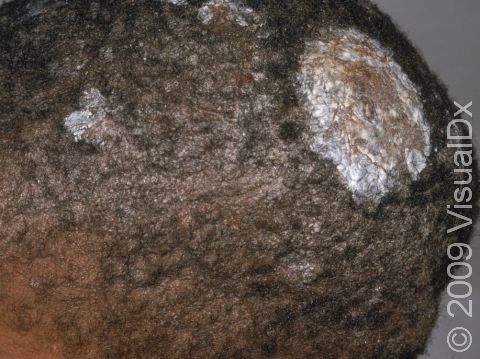
Scalp Ringworm (Tinea Capitis)
Tinea capitis is a fungal infection of the scalp, commonly known as scalp ringworm. Typically, the hair follicle becomes infected, and a small, scaly plaque (a raised area of skin larger than a thumbnail) appears. This can spread outward in all directions, causing a large, scaly, circular lesion. The hair that is involved usually becomes brittle and broken. If the scalp ringworm is left untreated, the scalp can become soft and very tender as the infection spreads. Children with scalp ringworm may have fever and pain along with enlarged lymph nodes.
Who's At Risk?
Although the typical age that children become infected is 3-7 years, infants can become infected, especially if other members of the household have a ringworm infection. Spores from the fungus may be airborne and spread easily. Direct contact through sharing of items such as combs and hats or from household items such as bedding and furniture also spreads the spores of the fungus.
Signs & Symptoms
Scalp ringworm appears as one or more round or oval plaques covered with gray scale and is often accompanied by hair loss. In lighter skin colors, the border can be pink or red, whereas in darker skin colors, it can be dark red, purple, brown, or grayish. Small pustules (pus-filled bumps) may appear, as well as tiny black dots on the surface of the scalp from broken hairs.
Lymph nodes at the back of the scalp, behind the ears, or along the sides of the neck may be swollen. Scalp ringworm is usually itchy.
One complication of scalp ringworm is a kerion, a thick, “boggy” or “mushy” nodule (a solid-raised bump that is firm to the touch) or plaque (a raised or bumpy area larger than a thumbnail) on the skin. If not treated aggressively, a kerion can lead to scarring and permanent hair loss.
Self-Care Guidelines
There are no effective self-care measures to treat scalp ringworm.
To prevent scalp ringworm:
- Have your child avoid close contact with infected people and pets.
- Have your child avoid sharing combs, brushes, hats, and hair accessories with friends and household members.
Treatments
To confirm the diagnosis of scalp ringworm, the medical professional may scrape some scales onto a slide and examine them under a microscope. This procedure, called a KOH (potassium hydroxide) preparation, allows the medical professional to look for signs of fungal infection.
Sometimes the medical professional will also perform a skin culture to document the presence of fungus or to discover the particular fungus that is causing the scalp ringworm.
Scalp ringworm is treated with oral antifungal medicines because the fungus invades deep into the hair follicle, where topical creams and lotions cannot penetrate. Scalp ringworm usually requires at least 6-8 weeks of treatment with an oral antifungal, possibly coupled with a medicated shampoo.
Visit Urgency
See a medical professional if your child has hair loss or itchy, scaly spots on the scalp.
If a close contact of your child (eg, a sibling or classmate) is diagnosed with scalp ringworm, make sure you examine the child’s scalp, looking for scaly spots. If you are suspicious about an area, seek medical care for an examination.
If your child is diagnosed with scalp ringworm, have any household pets evaluated by a veterinarian to make sure they do not also have a fungal infection. If the veterinarian discovers an infection, be sure to have the animal(s) treated.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on June 17th, 2024 at 4:37 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder