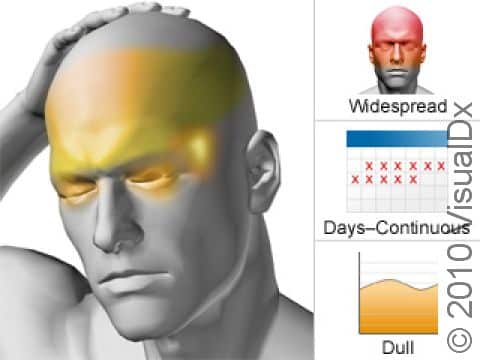
Chronic Tension Headache
Tension headache typically involves on-and-off head discomfort that is described as mild to moderate. It may feel like a nonthrobbing “tightness” or “pressure,” often on both sides of the head. People with a tension headache find they can usually go about their regular daily activities. Unlike with migraine, nausea, vomiting, and light and sound sensitivity are uncommon.
Tension headaches last from 30 minutes to several days. When tension headaches occur 15 times or more a month, they are considered chronic tension headaches.
While tension headaches are quite common (affecting about 30%-78% of the population), chronic tension headaches are much less common (affecting only about 2% of the population).
Who's At Risk?
Chronic tension headaches are slightly more common in women than men. People who take pain relievers too frequently for tension headaches are more prone to developing chronic tension headaches. People with fatigue, stress, depression, and anxiety are also at higher risk of chronic tension headaches.
Signs & Symptoms
With chronic tension headaches, unlike with migraines, there is no pulsating sensation and no necessity to lie still in a quiet, dark room. People with chronic tension headache do not usually need to stop what they are doing, noting that the headache is a nuisance but not incapacitating. It often involves large portions of the head, frequently the back of the head and neck, and involves a band-like sensation of pressure in these areas.
Self-Care Guidelines
Many people with tension headaches take over-the-counter pain relievers such as ibuprofen (eg, Advil, Motrin), naproxen (eg, Aleve), or acetaminophen (eg, Tylenol). These medications typically work well when the headaches first start, but when tension headaches become daily, they can contribute to worsening of the headache syndrome (see Medication Overuse Headache). For this reason, if headaches are 2-3 times or more a week, even over-the-counter medicines should be taken only after discussing them with your medical professional.
Self-care measures you can try include reducing stress, relaxation training, and biofeedback. Massage can also be effective. Good posture, practicing proper computer use, and limiting eye strain are all also important.
Treatments
Lifestyle changes are very important in treating tension headaches. The goal is to avoid headache triggers. Learning about tension headaches, knowing what to expect, and keeping in touch with your medical professional are key to success in controlling symptoms.
In chronic tension headache, a variety of contributing factors should be addressed, including:
- Anxiety and depression.
- Frustration.
- Physical and emotional dependencies.
- Factors such as obesity, snoring, poor diet, poor sleep habits.
- Medication overuse.
Some treatment options include:
- Relaxation therapies, hypnosis, and biofeedback.
- Monitoring your diet for triggers and eliminating caffeine.
- Improving sleep habits.
- Exercising regularly.
- Cognitive behavioral therapy, which is talk therapy with a trained counselor, designed to identify stressors and develop coping strategies to minimize their effect on behavior.
- Counseling and treatment for depression and/or anxiety.
- Physical therapy.
Your medical professional may prescribe preventive medication for chronic tension headache. If these are not effective, your medical professional may prescribe a migraine-preventive or other medications.
Visit Urgency
If your headaches are frequent enough to be considered chronic (ie, you have headaches 15 or more days per month), contact your medical professional. Also see your medical professional if you find you need to take over-the-counter medications more than 2-3 times per week because this can cause medication overuse headaches.
You should call your medical professional for any headache if:
- You develop new symptoms not typical of prior headaches.
- An unusually severe headache occurs.
- You feel disoriented or lose consciousness.
- Your headache lasts longer than 3-4 days (unless this is typical for you).
- Your headache wakes you up from sleep.
Immediately seek medical attention if you or someone you are caring for experiences:
- A stiff neck and a high fever with a headache.
- Loss of motor function (eg, your muscles don’t move normally), inability to think clearly, or convulsions with a headache.
- A head injury.
If you are currently undergoing treatment for chronic tension headaches, you should contact your medical professional if your headaches worsen, the quality of your headaches change significantly, or you develop side effects.
Last modified on October 7th, 2024 at 1:33 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder