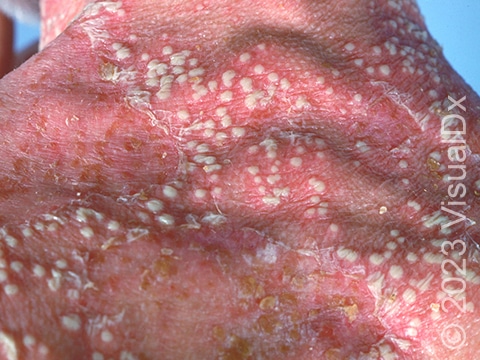
Generalized Pustular Psoriasis
Generalized pustular psoriasis (GPP) is an uncommon and severe type of psoriasis where many pustules (pus-filled bumps) develop on red, inflamed skin. Individuals with GPP often have other symptoms associated with their skin disease, such as a general unwell feeling, fever, itching, or skin pain. GPP may occur as a single episode or as a long-term condition that comes and goes for many years.
While the exact cause of GPP is unclear, it appears to be the result of an overactive immune system that attacks the skin. This subtype of psoriasis may occur in individuals with or without a prior history of plaque psoriasis. It may also occur in families, as several genetic causes of GPP have been identified. Flares of GPP can be triggered by infections, stopping topical steroids or other psoriasis medications, pregnancy, low calcium levels, certain medications, and other irritants to the skin, such as sunburns.
Who's At Risk?
GPP can affect people of any age, but it is most common in middle-aged adults, and it is more common in women.
Signs & Symptoms
GPP commonly appears as many similarly sized pustules covering large areas of skin, such as the trunk and arms and legs. Individual pustules may begin to merge into larger collections, sometimes referred to as “lakes of pus.” Pustules are often within red patches (flat areas of skin larger than a thumbnail) and may be more prominent around the edges of redness. The redness may be difficult to see in darker skin colors, where the patches may appear more purple, gray, or darker brown. The lining of the mouth can also be affected in GPP.
GPP differs from other types of localized pustular psoriasis, such as palmoplantar pustulosis. Nevertheless, people with GPP may have a personal history of plaque psoriasis. In this case, there may be pustules along with plaques (raised areas of skin larger than a thumbnail) covered by silvery scales, especially on the scalp, trunk, buttocks, genitals, elbows, or knees.
The lesions of GPP can become infected, and this condition may affect other organs in the body, such as the liver, joints, lungs, and kidneys.
Self-Care Guidelines
GPP is a severe type of psoriasis that can lead to serious complications if inadequately managed or treated. For this reason, there are no self-care measures that are adequate for treating GPP.
The National Psoriasis Foundation is an excellent resource for individuals with psoriasis, including GPP. Additional disease information can be found on their website at https://www.psoriasis.org/.
Treatments
The widespread redness and pus-filled bumps of GPP may mimic or resemble other pustular conditions or infections. Your medical provider may do a biopsy and skin culture along with some blood tests to rule out these similar conditions.
If you have severe GPP, your medical professional may recommend hospitalization to ensure appropriate care, including hydration, nutrition, temperature regulation, and treatment of any infection.
Initial management and general care from your medical professional may include:
- Topical steroids applied to the skin with damp dressings.
- Fluid replacement.
- Screening for infection.
- Other laboratory blood tests.
- Medications for pain management.
For ongoing care, your medical professional may prescribe the following:
- There is only one FDA-approved medication for GPP: spesolimab (Spevigo), which is an intravenous medication given for flares of GPP.
Other treatment considerations may include:
- Biologic medications such as ustekinumab (Stelara), secukinumab (Cosentyx), or ixekizumab (Taltz), depending on the age of the individual with GPP.
- Ultraviolet therapy, also known as phototherapy.
If you are pregnant or breastfeeding, you should discuss appropriate treatments for your GPP with a medical professional.
Visit Urgency
Concerning skin changes include widespread inflamed areas of skin and/or pus-filled lesions over patches of red skin or skin color changes. It is important to visit a dermatologist or seek urgent medical attention if you suspect you may have GPP.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on June 13th, 2024 at 11:21 am
Related Skin Conditions


Not sure what to look for?
Try our new Rash and Skin Condition Finder