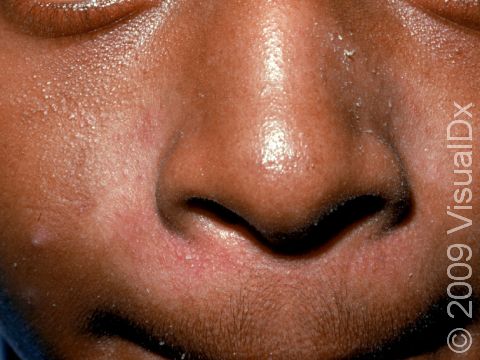
Seborrheic Dermatitis
Seborrheic dermatitis, also known as seborrhea, is a common noncontagious condition of skin areas containing oil glands (the face, scalp, and upper trunk). In seborrheic dermatitis, extra skin cells are produced (leading to flaking), and sometimes inflammation develops. This inflammation leads to pink or red colors in lighter skin colors or pinkish, purplish, dark brown, grayish, or whitish areas in darker skin colors, as well as itching. It varies in severity from mild dandruff of the scalp to scaly patches on the skin. A type of yeast normally found on the skin called Pityrosporum ovale lives in these oil-rich areas and plays a role in this condition. Seborrheic dermatitis seems to worsen with stress, dry weather, and infrequent shampooing. Although there is no cure for seborrheic dermatitis, you can usually control it with medicated shampoos and topical steroids (if inflammation is prominent).
Who's At Risk?
Children are more likely to have seborrhea in the first year of life and during the teenage years (adolescence).
Signs & Symptoms
The scalp is itchy and sheds white, oily skin flakes. One or more of the following areas may be involved:
- Scalp or hairline
- Forehead
- Eyebrows or eyelids
- Creases of the nose and ears
- Ear canals
- Breastbone
- Midback
- Groin or armpits
In lighter skin colors, seborrheic dermatitis patches may appear pink or red, and in darker skin colors, they may appear pinkish, purplish, dark brown, or grayish, or the affected areas may look lighter in color (hypopigmented).
Seborrheic dermatitis may be:
- Mild – only some flaking and skin color change (as outlined above) in a few small areas.
- Moderate – several areas affected with bothersome skin color change and itch.
- Severe – large areas of skin color change and severe itch that do not improve with self-care measures.
Self-Care Guidelines
Most cases of seborrheic dermatitis are easy to control with nonprescription home treatments. These include:
- Frequent shampooing or a longer lather time with shampoo. If a regular daily shampoo fails, consider an over-the-counter dandruff shampoo. There are several types on the market, and one may work better for an individual than another.
- Shampoos containing ketoconazole (Nizoral), selenium sulfide (Selsun Blue), 2% pyrithione zinc (Head & Shoulders), salicylic acid (Neutrogena T/Sal), or tar-based (Neutrogena T/Gel) compounds may be helpful. Consider occasionally rotating shampoos because the ability of how well a product works (its efficacy) can change with time.
- If the scalp is covered with widespread, dense scale, the scale may first be removed by applying warm mineral oil or olive oil to the scalp and washing several hours later with a detergent, such as a dishwashing liquid or a tar shampoo.
- Some over-the-counter creams will help if the medicated shampoo is not working well enough. These can be added to the shampoo until there is improvement and then can be discontinued; these creams can be used again temporarily as needed and include:
- Creams that reduce the Pityrosporum yeast (clotrimazole [Lotrimin], miconazole [Monistat]).
- Hydrocortisone (eg, Cortaid) cream, which may work well at first but may be less helpful if used for a long time.
- Managing eyelid inflammation (called blepharitis) by gentle cleaning of the skin around the eyelashes (eyelid margins) with a cotton swab and baby shampoo (eg, Johnson’s Baby Shampoo).
Treatments
- Corticosteroid creams, lotions, or solutions
- Sulfur or sulfacetamide products, such as a wash, cream, or lotion, applied on the skin (topically)
- Prescription-strength ketoconazole shampoo or cream
- Tacrolimus (Protopic) ointment or pimecrolimus (Elidel) cream
- Roflumilast foam (Zoryve) in children ages 9 years and older
Visit Urgency
See your child’s dermatologist or other medical professional if the condition does not improve with self-care measures.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on June 12th, 2024 at 4:56 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder