Plaque Psoriasis
Psoriasis is a common, noncontagious condition that can present in a variety of ways in the skin. The subtypes of this condition include plaque, inverse (or skin fold), guttate, erythrodermic, and pustular psoriasis. Plaque psoriasis, which represents approximately 85% of psoriasis cases, is a lifelong skin condition that affects about 2%-3% of the population worldwide. Plaque psoriasis skin lesions are typically red and raised with overlying scale. There may be papules (small, raised bumps) or plaques (larger, raised skin lesions that are bigger than a thumbnail), or both. People with plaque psoriasis typically have thickened, white scaly patches on their skin.
While the exact cause of psoriasis is unknown, this condition is the result of an overactive immune system that attacks the skin and other organs of the body. Psoriasis is very common in some families, suggesting a likely genetic component contributing to this disease, but it can also occur in individuals with no family history of psoriasis. Psoriasis can be triggered by certain environmental causes, such as emotional stress, pregnancy, injury to the skin, bacterial skin infections such as a streptococcal infection (“strep”), smoking or alcohol consumption, and ingesting certain medications.
Who's At Risk?
Plaque psoriasis can develop at any age, but it is usually diagnosed in the teenage or early adult years. Psoriasis may also occur for the first time in older adult patients between the ages of 50 and 70. Thirty percent of people with plaque psoriasis have a family member with plaque psoriasis. The condition affects men and women equally.
Certain medications can trigger flares of plaque psoriasis. These medications include beta blockers often used for high blood pressure, NSAIDs (eg, ibuprofen [Advil, Motrin], naproxen [Aleve]), lithium, antimalarial drugs, and oral steroids like prednisone. While TNF-alpha inhibitor medications (eg, etanercept [Enbrel], adalimumab [Humira], certolizumab [Cimzia], infliximab [Remicade, Renflexis]) are a known treatment for plaque psoriasis, these medications can sometimes cause plaque psoriasis in people taking these medications for other conditions, such as rheumatoid arthritis or Crohn disease.
Approximately one-third of people with plaque psoriasis also develop psoriatic arthritis, an inflammatory joint condition that causes painful, swollen joints and can lead to irreversible joint destruction. Importantly, individuals with psoriasis are also at increased risk for other health conditions, such as heart disease, stroke, high blood pressure, diabetes, obesity, sleep problems, anxiety / depression, social stigma, cancer, and even death.
Signs & Symptoms
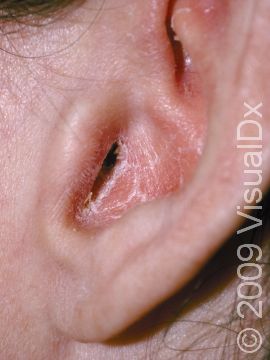
The typical lesions of plaque psoriasis are raised patches of irritated skin that are often covered with a thick, white scale. In lighter skin colors, the patches are most often pink or red. In darker skin colors, the redness may be harder to see or may appear purple, grayish, or dark brown.
Psoriasis plaques are most frequently seen on the elbows, knees, trunk, buttocks, belly button, palms / soles, and scalp. The skin lesions are usually found on both sides of the body (symmetrically). Skin areas of physical trauma or friction may develop psoriasis plaques, which is why the hands / feet, scalp, knees, and elbows are commonly affected. Body folds such as the genitals or underarms may also be affected but tend to lack the classic thick, white scale often seen in other body locations. Most individuals experience itching or skin / joint pain, but some may not.
Plaque psoriasis is commonly categorized by disease severity in the following way:
- Mild psoriasis – Few, scattered, limited areas of involvement that account for less than 10% of the body. To generally estimate body percentage involvement, the surface of a person’s palm print represents approximately 1% of their body surface area (ie, 3 palm prints of psoriasis lesions on the body is equal to approximately 3% of their body surface area). Topical or ultraviolet-based therapies are commonly used to treat mild psoriasis.
- Moderate-to-severe psoriasis – More widespread disease affecting larger areas of the body and account for at least 10% of the body. Individuals with these more severe forms of psoriasis often require more aggressive medical treatments in addition to or in lieu of topical therapies.
- Special considerations – Categorizing psoriasis solely on the percentage of affected skin has important limitations. Individuals with psoriasis who have pain in the joints and/or involvement of certain skin sites (hands / feet, scalp, genitals, or face), even if the overall percentage is less than 10%, may require more aggressive treatment beyond topical medications due to the impact psoriasis can have when involving these special sites of the body.
Other symptoms of psoriasis can include inflammation of tendons or ligaments, swollen fingers or toes, hair loss (alopecia), eye irritation (uveitis), or changes in the nails. Nails of the hands or feet may develop tiny pits or indentations, yellow-brown spots, or lifting up of the nail from the nail bed (onycholysis).
Importantly, plaque psoriasis if often confused with other skin conditions that can look similar, such as fungal infections of the skin, eczema (atopic dermatitis), allergic reactions, or irritation of skin exposed to specific environmental materials or products. Your medical professional may be helpful in determining the cause of your skin rash if the diagnosis is unclear.
Self-Care Guidelines
Because plaque psoriasis is a lifelong, chronic condition that currently has no cure, the goal of treatment is to decrease the number of skin lesions and reduce symptoms such as itching and pain. Most beneficial treatments for plaque psoriasis work in part due to their ability to alleviate the body’s abnormal immune attack of the skin and help prevent the excessive buildup of skin cells or flakes.
- Bathe daily to help soften scales and moisten the skin. Avoid harsh soaps and scrubbing the skin as these may worsen psoriasis. Moisturizing soaps and soap substitutes, such as unscented Dove Sensitive Skin Beauty Bar, Vanicream Cleansing Bar, and CeraVe Psoriasis Cleanser, are milder products for the skin.
- The application of moisturizers after water exposure or bathing may be helpful. Heavier oil-based moisturizers help to retain water in the skin better than water-based moisturizers. Thicker moisturizers such as petroleum jelly (Vaseline), Aquaphor Healing Ointment, Eucerin Original Healing Cream, Vanicream, Aveeno Moisturizing Cream, CeraVe Healing Ointment, or CeraVe Moisturizing Cream can be applied to damp skin daily after bathing. Use cream and ointments rather than lotions because lotions can dry out the skin.
- Apply over-the-counter hydrocortisone cream or ointment (0.5% or 1%) twice daily for 2-3 weeks at a time to help reduce itch and irritation. Stronger topical steroids are typically required for thicker psoriasis plaques. Long-term use of topical steroids should include periodic times of no treatment each month to avoid thinning of the skin.
- Use of products with salicylic acid (shampoos, cleansers, and ointments), such as Neutrogena T/Sal, can help soften and remove thick psoriasis scale in the scalp.
- Small doses of natural sunlight may be helpful, such as 10-15 minutes approximately 2 or 3 times per week. Avoid too much sun; however, and protect your healthy skin from excessive sun exposure to help prevent premature aging of the skin and skin cancers.
- Follow a healthy diet to maintain an ideal weight. (Being overweight may make plaque psoriasis worse.)
Patient Support Resources
The National Psoriasis Foundation is a useful resource for patients and health professionals that has additional information regarding psoriasis and the various available treatments. The National Psoriasis Foundation website includes access to psoriasis-related articles, psoriasis research, a directory of health care professionals with an expertise in psoriasis, and opportunities for patients to volunteer or get involved in upcoming events.
Treatments
There are many prescription-strength topical, oral, and injectable treatments that are helpful at controlling plaque psoriasis. For localized or mild psoriasis:
- The most common therapy for plaque psoriasis is topical steroids, either in cream or ointment form. Low- or mid-potency steroids, such as hydrocortisone 2.5% or triamcinolone, may be useful for thinner areas of skin (face or eyelids) or more sensitive body sites (armpits or genitals). Higher-potency topical steroids, such as clobetasol, halobetasol, or betamethasone, are used for the scalp, trunk, and extremities. Steroid solutions, foams, or liquids are very helpful for the treatment of scalp psoriasis. Use should be limited to twice-daily application for 2-3 weeks at a time followed by a 1-week break due to the possible development of stretch marks (striae) or thinning (atrophy) of the skin with long-term topical steroid use.
- Calcipotriene (Dovonex) is a nonsteroid vitamin D derivative cream that may help treat psoriasis plaques and is even more effective when combined with topical steroids.
- Tazarotene (Tazorac) is a vitamin A–based cream that may be prescribed to help reduce the inflammation, thickening, and scaling of the skin. Individuals of childbearing potential should avoid use in pregnancy as this class of medication may cause birth defects.
- Roflumilast (Zoryve) 0.3% cream is a nonsteroid cream approved for once-daily use in individuals aged 12 years and older and can be used safely on the face and skinfolds as well as other areas of the body.
- Tapinarof (Vtama) 1% cream is another nonsteroid cream approved for once daily use, but it is only approved for adults with plaque psoriasis.
- Coal tar–based therapies and anthralin (Drithocreme) creams are sometimes used, but they are used less frequently than other treatments because they have a foul odor, cause skin irritation, and can stain clothing, and because neither is any more effective than calcipotriene.
Treatment for moderate-to-severe psoriasis or plaques involving special skin sites:
- If a large percentage of your skin is affected, ultraviolet (UV) light therapies may be considered. These include UVB phototherapy and PUVA (psoralen [a photosensitizer] and UVA therapy). PUVA may increase your risk for nonmelanoma skin cancers and may be less effective in darker skin colors.
- Injected (subcutaneous) or intravenous biologic therapies are one of the most common medications used for plaque psoriasis. These are proteins that treat plaque psoriasis by blocking certain abnormal immune signals of the immune system that cause psoriasis. This class of medications is highly effective at treating psoriasis but may be costly if not covered by insurance. The number of injections each month and the side effects differ for each medication and should be discussed with your medical professional. Such medications include:
- TNF-alpha inhibitors (eg, etanercept [Enbrel], adalimumab [Humira], certolizumab [Cimzia], infliximab [Remicade, Renflexis])
- IL-12/23 inhibitor (eg, ustekinumab [Stelara])
- IL-23 inhibitors (eg, guselkumab [Tremfya], risankizumab [Skyrizi], tildrakizumab [Ilumya])
- IL-17 inhibitors (eg, secukinumab [Cosentyx], ixekizumab [Taltz], brodalumab [Siliq]).
- Deucravacitinib (Sotyktu) is a once-daily oral pill approved for the treatment of moderate-to-severe plaque psoriasis.
- Apremilast (Otezla) is an oral medication that is taken once to twice daily and is approved for the treatment of plaque psoriasis and psoriatic arthritis.
- Older oral medications may be used for the treatment of moderate-to-severe psoriasis, including acitretin (Soriatane), which is made from vitamin A, methotrexate, and cyclosporine (Gengraf, Neoral). If you are prescribed any of these medicines, you will need to see your medical professional regularly to monitor for possible side effects (such as liver and kidney damage) that may result from use of these medications.
All individuals who are of child-bearing potential, pregnant, or breast-feeding should discuss the safety of all available psoriasis treatments with their medical professional prior to use.
Visit Urgency
Individuals with psoriasis should see a medical professional such as a dermatologist or rheumatologist if self-care measures are not helpful, if the psoriasis is widespread, or if there is joint or bone pain in the setting of psoriasis.
Individuals with psoriasis are also at increased risk for other health conditions such as heart disease, stroke, high blood pressure, diabetes, obesity, sleep problems, anxiety / depression, social stigma, and cancer. See a medical professional to help screen for these conditions if you have psoriasis.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on June 13th, 2024 at 4:18 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder